The purpose of the Patient History Form of a patient is information gained by a physician by asking specific questions, either of the patient or of other people who know the person and can give suitable information, with the aim of obtaining information useful in formulating a diagnosis and providing medical care to the patient. The information obtained in this way, together with the physical examination, enables the physician and other health professionals to form a diagnosis and treatment plan.
From the Diary click on
Clinical >> Patient History Form- Presenting Complaint: History of the present illness. Following the chief complaint in medical history taking, a history of the present illness refers to a detailed interview prompted by the chief complaint or presenting symptom (for example, pain).
- Past Medical History: In a medical encounter, a past medical history, is the total sum of a patient's health status prior to the presenting problem.
- Pregnancy/Birth History: It is important to ask about a female patient's previous obstetric history, as this can often help inform the assessment of risk in the current illness/pregnancy and have implications for the mode of delivery.
- Feeding/Diet: A dietary history is a structured interview method consisting of questions about habitual intake of foods from the core (e.g. meat and alternatives, cereals, fruit and vegetables, dairy and 'extras') food groups in the last seven days.
- Growth and Development: Growth is the progressive increase in the size of a child or parts of a child. Development is a progressive acquisition of various skills (abilities) such as head support, speaking, learning, expressing the feelings and relating with other people. Growth and development go together but at different rates.
- Immunization: Immunization is the process whereby a person is made immune or resistant to an infectious disease, typically by the administration of a vaccine. Check and take note that the patient is currently up to date with their vaccinations:
- Flu vaccination
- Whooping cough vaccination
- Hepatitis B vaccination (if at risk)
- Family History: Taking a brief family history can help to further assess the risk of adverse outcomes to the Patient. This can also help inform discussions with patients about the risk of having a specific genetic disease (e.g. cystic fibrosis).
- Social History: Understanding the social context of a patient is absolutely key to building a complete picture of their health. Social factors have a significant influence on a patient’s health and it’s therefore key that a comprehensive social history is obtained.
- Other: Any other relevant information to the patient or notes the Doctor wants to make.

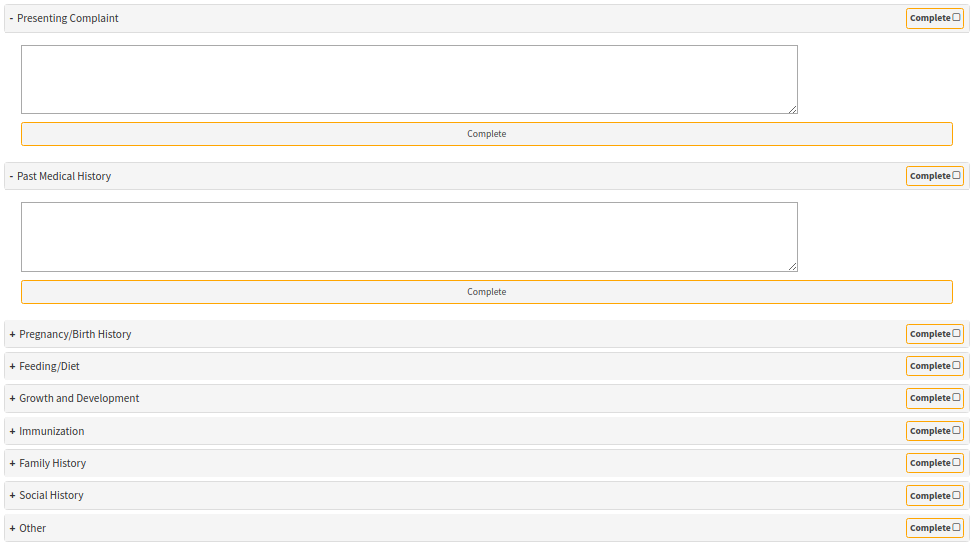
- If you click on a panel to complete the section, it will expand. All fields are Free Text.
- Once you are done taking notes, click on Complete.
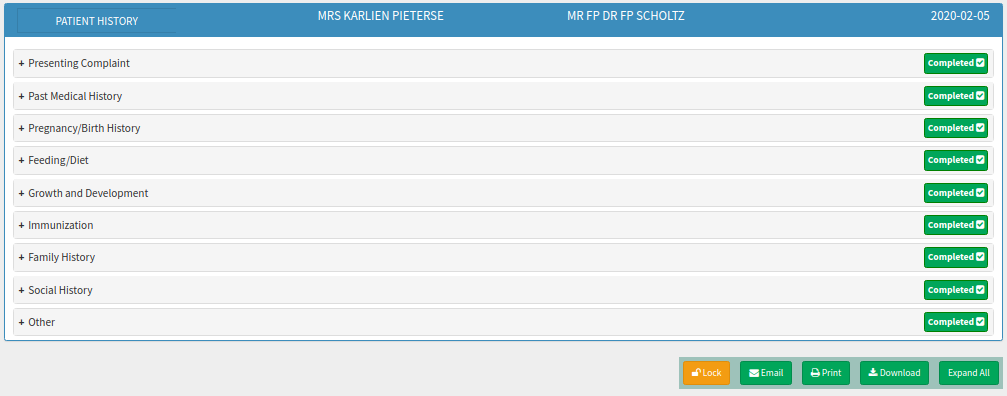
- If all sections are completed it will turn Green with a correction mark in the tick box.
- From here you can Email / Print or Download the Form in CSV or pdf format.
Last modified: Thursday, 21 December 2023, 11:03 AM