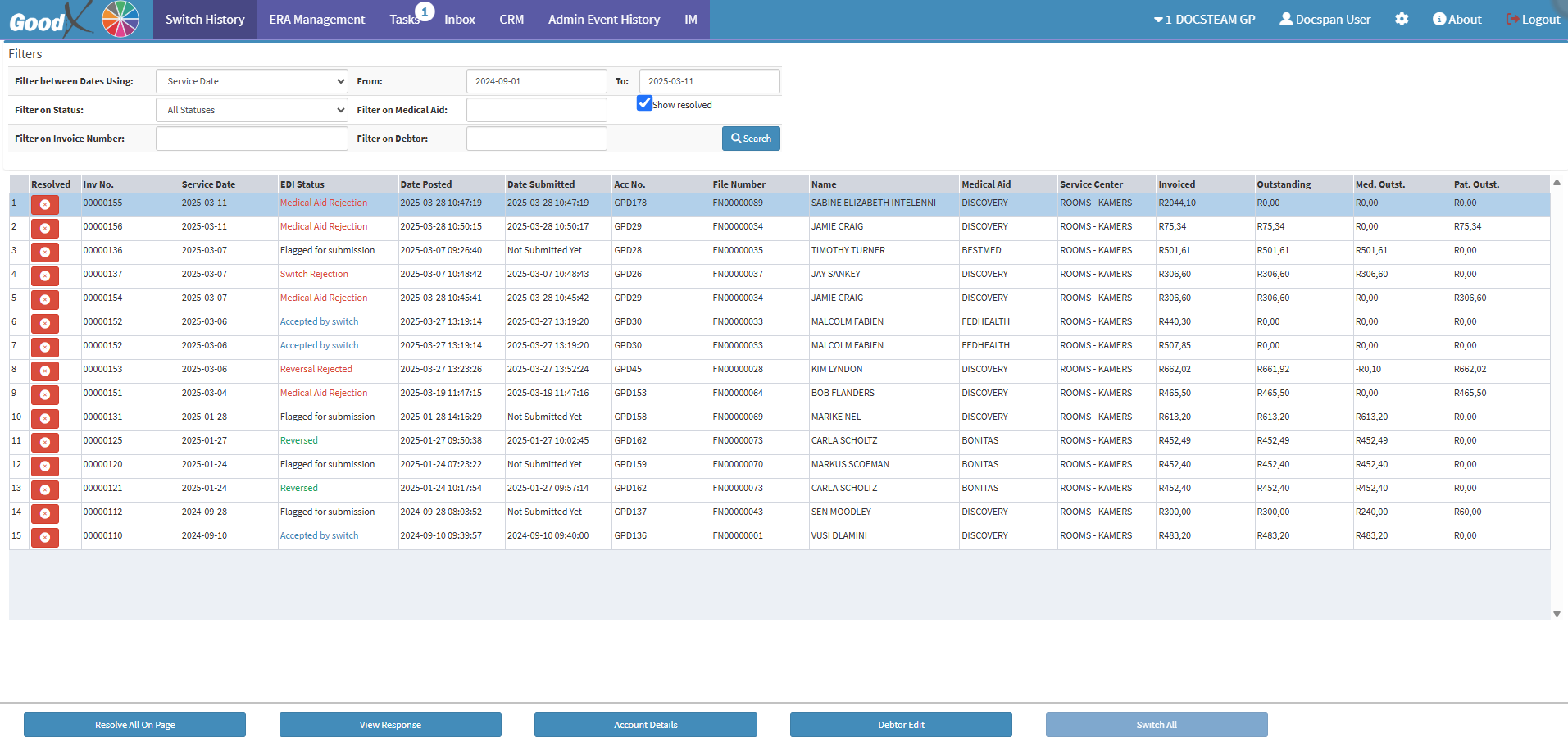
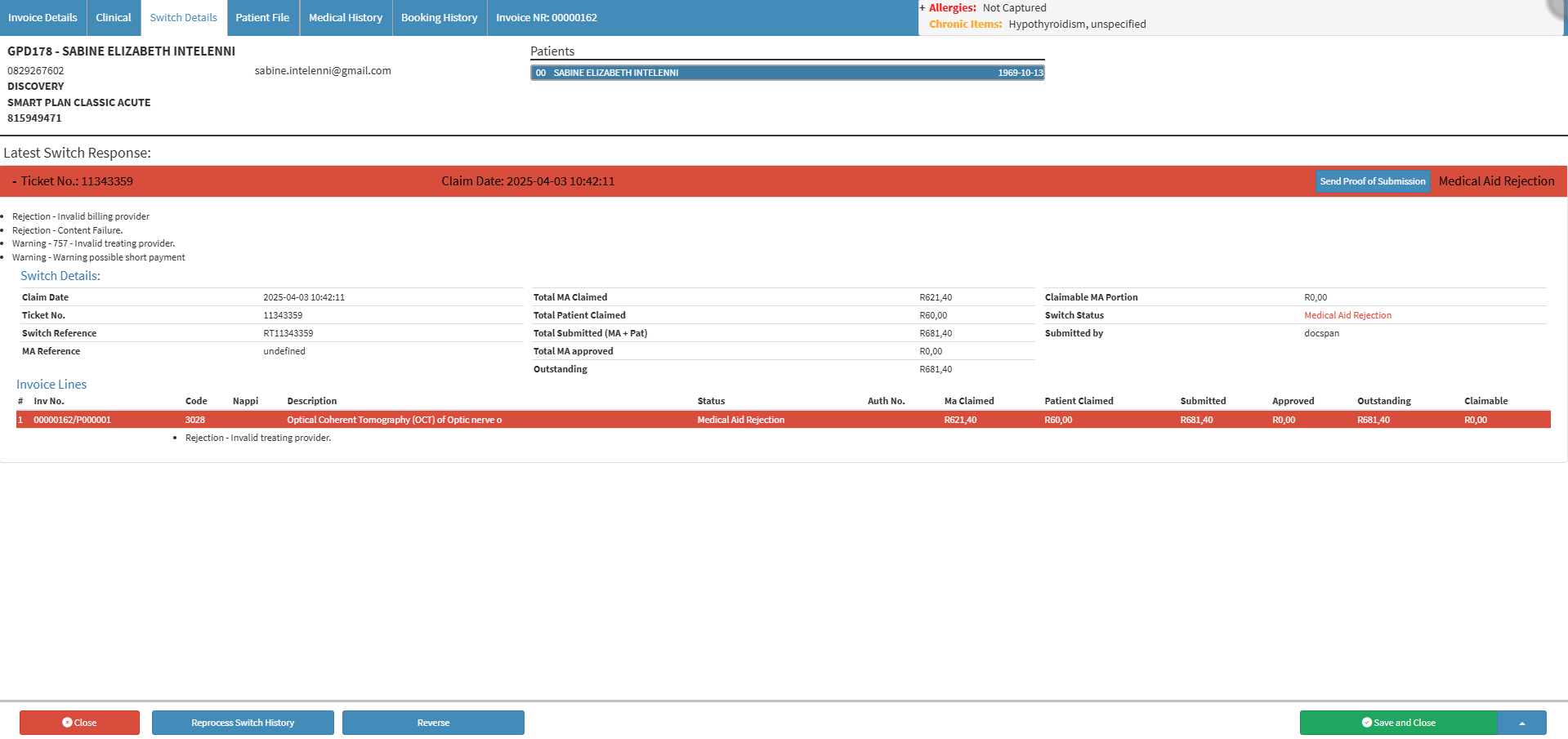
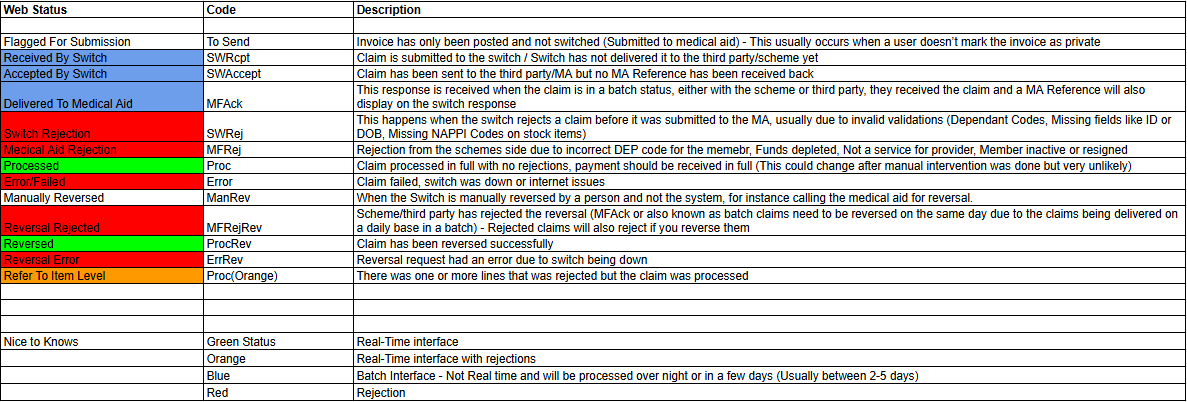
The EDI Response is essential for confirming whether a claim submitted to a Medical Aid will be paid or rejected. It helps the Practice quickly identify approved, partially approved, or declined claims, reducing delays in payment processing. By reviewing the EDI Response, you can take immediate action on any issues, ensuring accurate billing and maintaining smooth cash flow for the Practice.
Text size
Line height
Text spacing