Best Practice Guidelines: Telehealth Practice Management
Copyright © 2020 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
6. Consultation phase
6.5. Treatment Plan
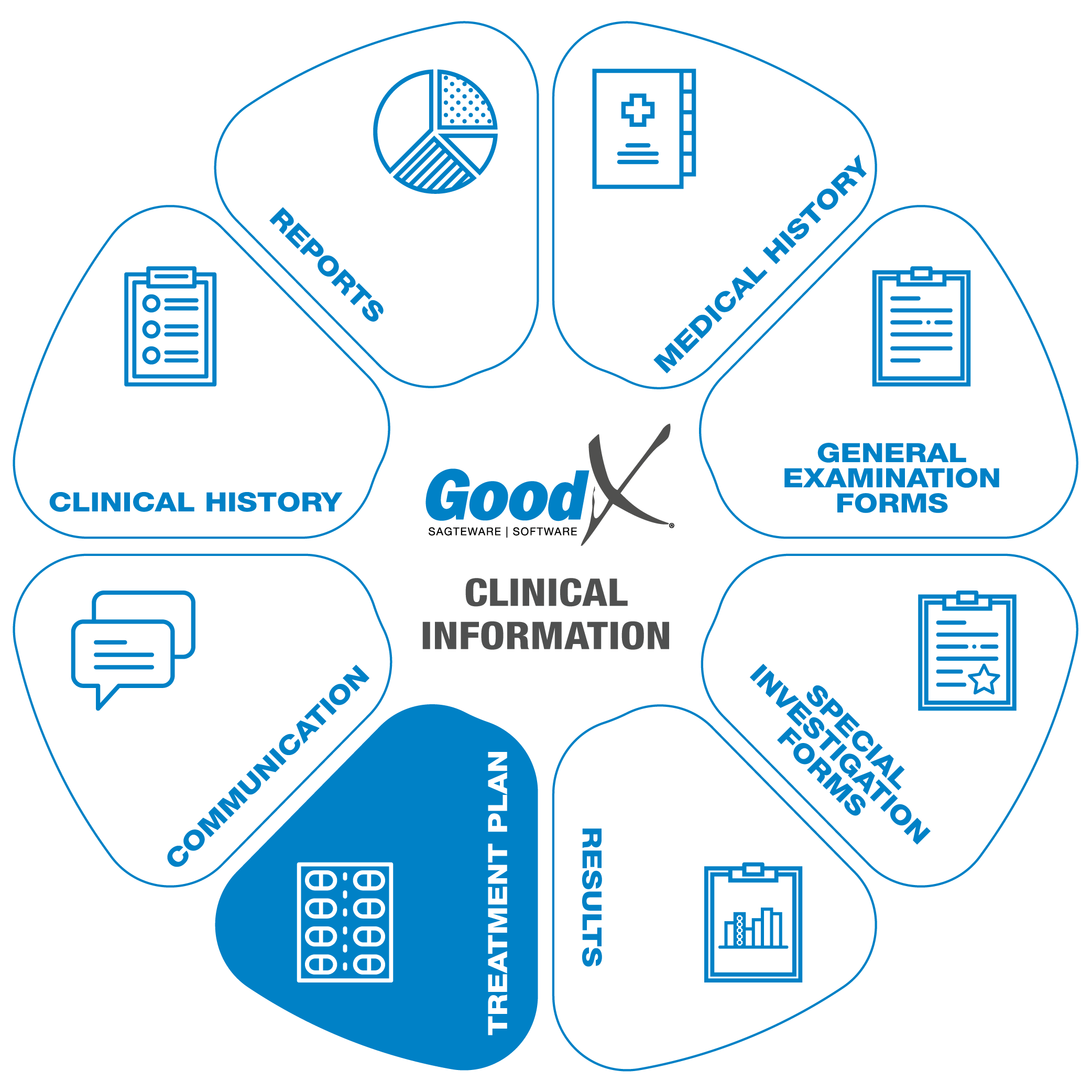 A treatment plan contains
details about the patient’s condition, as well as the practitioner’s recommended treatment.
A treatment plan contains
details about the patient’s condition, as well as the practitioner’s recommended treatment.
During this part of the consultation, the patient's diagnosis will be discussed and documented. Possible treatment plans and recommended next steps will then be discussed with the patient. Once you have discussed the patient’s options, you can complete your diagnosis and treatment plan documentation. Furthermore, any necessary auxiliary documentation can be created such as scripts and medical certificates (sick notes).
The following information should be uploaded into your software or kept there for future reference:
- The diagnosis and suggested treatment plan alongside the general examination documentation
- General notes about the patient’s condition
- Documentation of procedures and materials billed
- Referral letters and
- All files and notes relating to the treatment plan
- Scripts:
- Acute and chronic scripts will be kept for record purposes.
- Chronic scripts will link chronic conditions to the patient’s file, and quick scripting will allow the practitioner to access previously used medications and chronic scripts.
- Acute and Chronic scripts will be saved to the patient’s medical history.
- Medical certificates:
- Will be created for the patient’s employee, school or university.
- A practitioner can also create family responsibility certificates so that e.g. a father can stay home to take care of his daughter.
- A practitioner can also provide travel certificates for their patients during the Covid-19 lockdowns.
Some of the Treatment Plan or Clinical Forms available in GoodX:
Authorisation Setup
For certain procedures or treatments, the patient will need authorisation from their medical aid to proceed with the treatment or procedure.
The authorisation number received from the patient's medical aid will be an indicator that the medical aid will pay for the procedure or treatment that they’ve agreed upon.
When the Authorisation number has been received the authorisation can be set up on the patient's electronic file, to pull through to the billing and go through to the medical aid when the invoice is switched.
The authorisation number must be included in the billing to ensure payment from the medical aid.
Scripts
Scripts will allow the patient to get the necessary medication to aid in his/her treatment from any pharmacy. The script can be emailed to some pharmacies depending on the schedule of the medication. The patient can collect the medication from the pharmacy or arrange that the medication be delivered to their home.
The script form has a lot of features that make scripting a quick and easy process, the practitioner can decide which features suit their workflow the best. Following: An explanation of some of these features:
Acute scripts
The most basic script that can be created is an acute script. An acute script consists of a list of short term medications with directions of use and diagnosis.
Directions builder
Every script line has a direction builder that assists the practitioner in creating directions of use for each script item. The direction builder allows the practitioner to populate the directions field, by selecting options from some dropdowns (e.g. time of day, meal relationship and route) and entering numbers in some fields (e.g. dosage, frequency and days supplied).
Chronic scripts
Chronic scripts are scripts that contain chronic items. An item can be marked as chronic by either manually marking the item as chronic or by marking the item as more than five times repeatable. When a script as a whole is marked as more than five times repeatable all of the script items will be marked as chronic.
Script history
The practitioner can quickly recreate any formerly scripted script line or script from the patient’s script history which is displayed at the bottom of the script.
Script favourites and macros
When creating a script the practitioner can save a script item with its directions of use as a favourite or save a couple of script items as a macro. When creating a script the practitioner can easily add script items, by adding favourites/macros to the script.
Import chronic lines
Another way to quickly create script lines is to import script lines from the medical history, where you can setup a script per chronic condition for each patient.
Generics
On every script line, the practitioner can quickly view generics for the selected script item and easily replace the script item with a generic.
MIMS
Practitioners can easily view the MIMS info for a selected script item.
Drug interaction checker (DIC)
While a script is being created the drug interaction checker checks for interactions between all of the scripted items and warns the practitioner about interactions. The practitioner can also open the DIC on the script to see more information about the interactions, as well as to see information about the side effects of the medication and the directions of use for each medication.
ConsumablesConsumables can be included in the script.
Electronic signature
The practitioner can sign the script electronically, or import their signature from the settings onto the script by using their pin that they set up in the settings along with the signature.
Add script lines to an invoice
When the practitioner is done with the script, they can add the script lines to the invoice.
Medical Certificate (Sick Note)
Sick notes are used to indicate that the patient has a certain condition and also as a declaration that the patient is unfit to continue with their normal daily routine or responsibilities for a specified period of time. The sick note can be completed and signed electronically by the medical practitioner. At the top of the sick note form, a record of the patient’s previous sick notes is displayed as well as the patient’s details. The following functions on the sick note will assist in creating the sick note with all the necessary information:
- Patient details will be filled in from the booking that was made
- Previous sick notes will be displayed
- ICD10 can be chosen from a list
- Diagnosis can be set to display on the printout
- The diagnosis that will be displayed on the printout can be modified
- Date of treatment (by default set to appointment date) can be set
- The absent from date will default to the appointment date and can be modified
- Number of days absent field
- Absent to and including date field. This field can manually be set or automatically updated by changing the number of days absent field
- A follow-up date can also be set
- Light duty from a specific date
- Light duty to a specific date
The practitioner can select one of the following statements to be added to the sick note:
- According to their opinion/knowledge or according to what they were informed by the patient, if the last option is chosen the patient’s signature can be captured
- The activities/responsibilities that the patient is unfit for can be selected from the following list: work, school, sport, university/college, travel
The practitioner can also create a family responsibility certificate for a family member.
The practitioner can sign the sick note electronically or import their signature from the settings onto the sick note by using their pin that they set up in the settings along with the signature
All the completed information will be compiled into a short story on the printed sick note with all the information that was added to the sick note.
The patient can also request a Travel certificate, for example
- Medical reasons to anther Country
- Healthy enough to travel for work or pleasure.
Referral letter
A referral letter is a form that can be completed when the patient has to be referred to another medical practitioner, for additional or special treatment that the current practitioner cannot perform. The referral letter contains the following features:
- Date of referral (default date is the appointment date)
- Referring note (free text field)
- Patient at practice since (when did the current treatment start)
- Doctor signature
- Diagnosis details (chronic, previous and reason for referral)
- Specialist details (name, practice number, address)
- Appointment details (date, time and location details)