Best Practice Guidelines: Telehealth Practice Management
Copyright © 2020 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
6. Consultation phase
6.1. Medical History
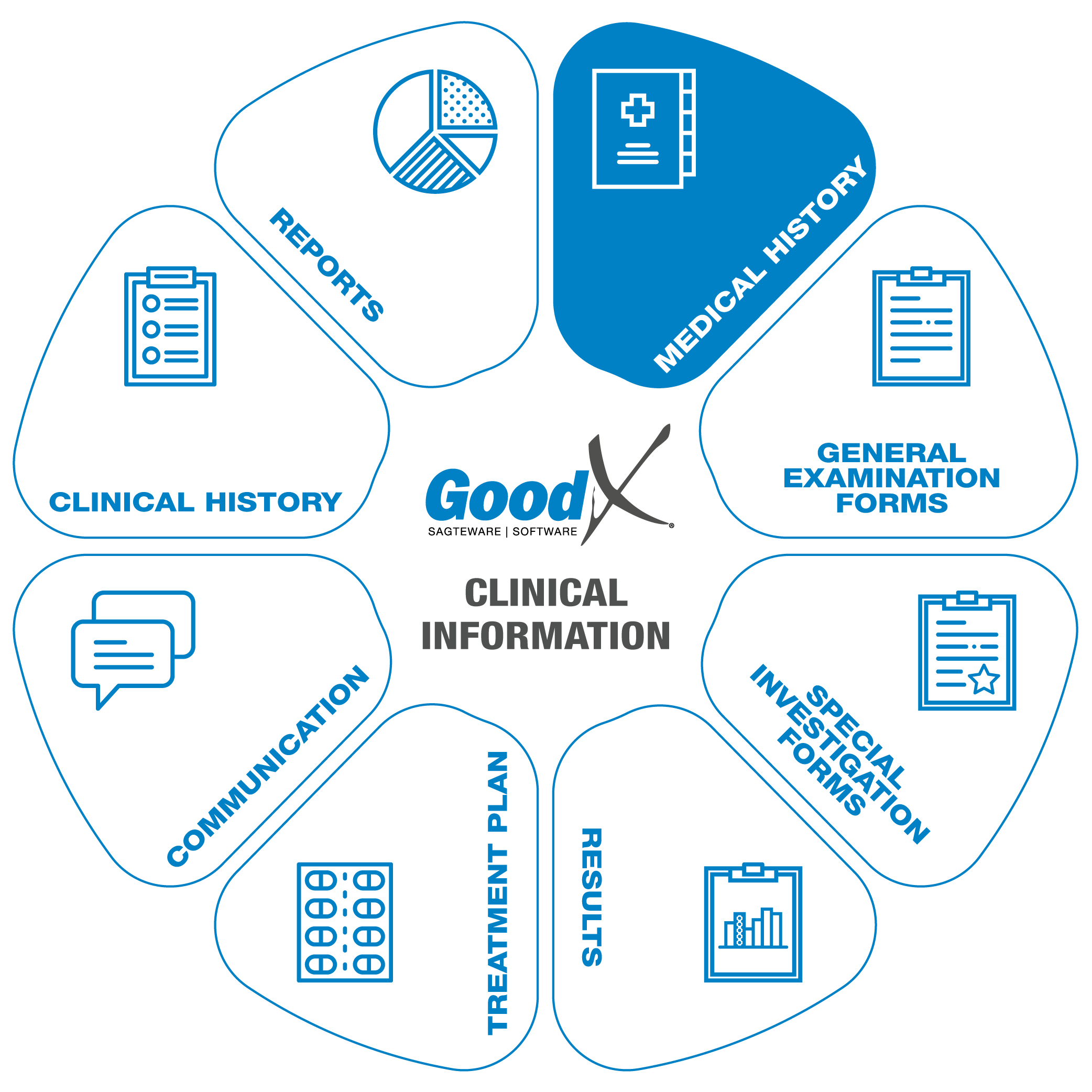 The medical history will
usually be completed during the first consultation with a patient and updated at each subsequent consultation. This will assist the medical practitioner to effectively treat and manage their patient’s health.
The medical history will
usually be completed during the first consultation with a patient and updated at each subsequent consultation. This will assist the medical practitioner to effectively treat and manage their patient’s health.
The practitioner will receive a warning if potential harmful actions are taken such as prescribing medication that the patient is allergic to. This will only happen if the patient's medical history has been completed on GoodX in full.
Completing the medical history also streamlines the practitioner’s workflow, for example, chronic scripts can be set up for a patient and then every time the patient needs a repeat chronic script, the practitioner can easily recreate the script.
Discuss any pre-consultation questionnaire results with the patient during this process if you have not done so prior to the consultation.
You can also review a patient’s clinical history with your practice during this part of the consultation as it will give you some extra context of the patient’s condition which you can use throughout the consultation to help with diagnosis and treatment planning as well as interpreting special investigation medical reports.
Capturing a patient’s medical history during a Telehealth consultation doesn’t need to be done differently than an in-person consultation; it is, however, convenient to use a platform which allows you to both capture medical information and have a Telehealth consultation in one place.
Relevant medical history to be checked includes:
- General information, for example, the patient's health habits like smoking, alcohol consumption, exercise and any other general information that you need to be aware of.
- Also, check the patient’s Family history.
- Past and current chronic conditions and any medication used currently or in the recent past.
- Allergies/intolerances and any relevant notes
- If it is relevant to the consultation, the operation, vaccination and travel history of the patient can also be discussed.
Medical History
The medical history comprises the following information:
General History
General Health
In this section, some of the patient’s habits (e.g. How often they smoke, drink alcohol, exercise and use recreational drugs) can be captured and their general well being can then be assessed. This information is also displayed in the medical history summary which is visible from all screens of the patient booking.
Family History
Here the practitioner can record the patient’s family medical history i.e. what chronic conditions and major medical events family members have experienced. For example Cancer, Hypertension, Asthma, Strokes, etc. Practitioners can use this information to help patients manage their health risks by suggesting that patients take certain actions. Knowing a patient’s family medical history can help practitioners with early diagnosis of serious conditions that the patient may be at risk of developing by checking for signs of the conditions regularly.
Chronic
This section is used to keep track of the patient’s chronic conditions and when the patient was diagnosed with each condition. A script template (i.e. medications, directions for use, dosages, etc.) can be created for each chronic condition that the patient is diagnosed with so that the practitioner can quickly and easily recreate a chronic script for the patient. This information is also displayed in the medical history summary which is visible from all screens of a patient booking.
Allergies
A patient’s allergies can be recorded here. A warning message will be displayed whenever the practitioner creates a script/invoice containing an item that the patient is allergic to. This information is also displayed in the medical history summary which is visible from all screens of a patient booking. The Allergies section consists of the following features:
No Allergies
If a patient has no allergies it can be noted on their medical record.
Message
A message can be added to a patient’s medical history which will be displayed in the medical history summary which is visible from all screens of a patient booking. This message can also be marked as important which means it will be displayed in a popup message whenever any of the booking screens are opened for that patient. For example, a message could be set up to remind the practitioner of the patient’s severe reaction to a certain allergen.
Allergens
The allergens are divided into three categories. In each of the categories the patient’s allergies can be recorded by the type of allergy and a message can be added to each recorded allergen. The allergens are divided into the following three categories:
- Drug Classes: Here is a list of drug classes that a patient could potentially have a severe immune response to. A drug class is a set of medications and other compounds that have similar chemical structures, the same mechanism of action (i.e. bind to the same biological target), a related mode of action, and/or are used to treat the same disease.
- Natural Allergies: This list contains natural allergens such as eggs, nuts, or dust. Natural allergens are products that contain any substance produced by life.
- Chemical Allergies: This list contains chemicals that can cause an allergic response. In this section, the practitioner can search for chemical allergens by medication i.e. the patient knows they are allergic to Panado thus the practitioner can search for Panado in the Search by medicine field and the system will show a list of all the chemical allergens contained in Panado e.g. paracetamol.
Treatment History
This section contains a list of treatments that the patient has had. The following information can be recorded per treatment:
- Treatment description
- Start date
- End date
- Place of treatment
- Dr notes - such as observations during the treatment
Operation History
This section contains a list of operations that the patient has had. The following information can be recorded per operation:
- Operation description
- Operation date
- Doctor/Surgeon
- Hospital
- Notes - such as complications during surgery
Gynecological History
Past Pregnancies
This section contains a summary of the patient’s past pregnancies as well as a list of the details of each past pregnancy. The details of each pregnancy that can be captured are date, GA weeks, length of labor, birth weight, sex, anesthesia, place of delivery, delivery type, ectopic, multiple births, c-section, comments/complications. The summary contains the following information: total (full-term/preterm) pregnancies, total living, total spontaneous abortions, total inducted abortions, total ectopics, total multiple births, total c-sections.
Menstrual History
Here information about the last menstrual cycle is captured such as the duration, start date, and end date.
Genetics Screening/Teratology Counselling
This section contains information about the patient and their family, for example, mental retardation, recurring stillbirths, or down syndrome.
Infection History
If the patient has been infected with or exposed to certain infections (e.g. HIV, TB, or Syphilis) it can be recorded in this section.
Occupational and Demographic History
The patient’s occupation also plays a role in their health and thus it is important to know where the patient works and what the patient does for a living. In this section, the patient’s occupation can be captured as well as any additional notes about the patient’s occupational and demographical history.