Best Practice Guidelines: Hospital Patient Administration

Copyright © 2019 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
14. Claim Administration
Responsible Roles
 |
Sent the updated case management report to the medical aid with all supporting documents. Ensure that all queries from the medical aid were dealt with and sorted out. |
|---|---|
 |
Ensure all billing are up to date. Switch the claim to the medical aid by sending the claim electronically through real-life switching. Check the response, reverse and correct any rejections. Check the patient validations. |
 |
Check the bank statements or get the information from the financial manager for all payments from the medical aid. Allocate the payments that were received from the medical aid by posting the ERA. Only post the ERA when the payment has been received in the bank account. Post any EFT payments from the patients onto their account. |
 |
Supply the Debtors clerk with the payments that come in on the bank statements from the medical aids and any EFT's from patients. Check if all payments that were received into the bank account were posted. Sign off all credit notes that were done on the patient's accounts. |
 Purpose of Claim Administration
Purpose of Claim Administration
To send the account to the medical aid and claim the amount from the medical aid to be paid. The process will assist in the most efficient method of claim administration.
Send the claim to the medical by using a real-time submission to the medical aids. Check the response immediately and correct any mistakes and followup on the rejection reasons. Allocate the payment and resolve the claim.
Critical Steps of Claim Administration
Cash flow is of vital importance to the health of a practice. One way of optimising the cash flow is to send your claim through to the medical aid before the patient leaves the hospital so that the cashier will know if the medical aid will settle the account. Unfortunately, this is not always possible at hospitals.If the claim is rejected by the medical aid, the cashier can inform the patient and receive payment directly from the patient before he or she leaves the practice.
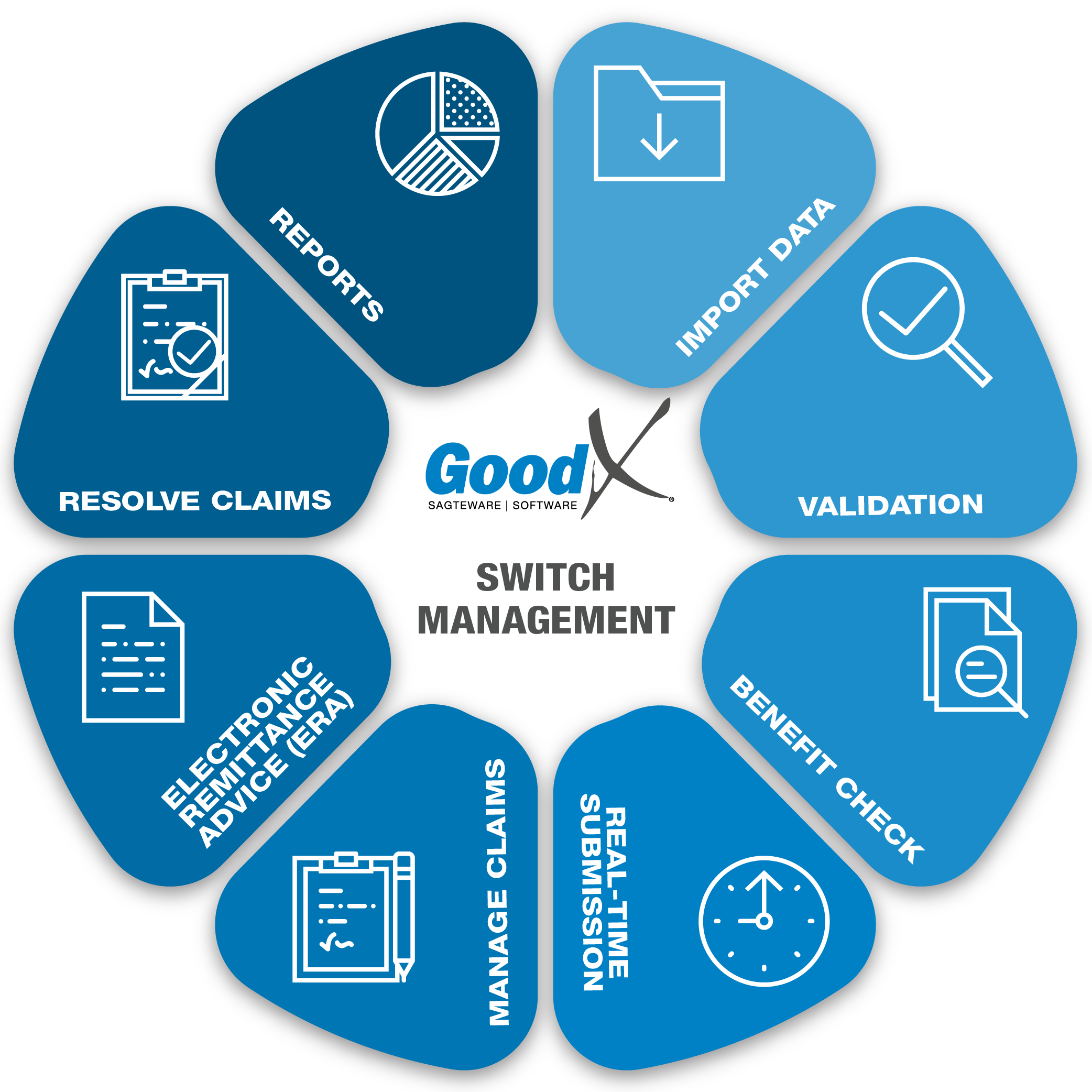
- The EDI process is followed directly after the billing and finalisation of the account:
- Ensure that there are no rejections.
- If any rejections, follow up on discrepancies, rectify and EDI again.

EDI process
Medical Aid patient accounts, when the file was audited the account must be sent through to the medical aid, with the electronic claim process.
- On GoodX Software the EDI process is one button to sent the claim to the medical aids.
- Wait for the response, correct any rejections immediately.
- Reverse the claim
- Resend the claim with the correct details.
- Wait for the next response until everything is corrected on the account.
- If the claim was rejected due to inefficient funds a statement can be handed to the patient as soon as possible to ensure immediate payment.
Manage Claims with an EDI History function
- Use the EDI History screen to manage the claims already send to the medical aids.
- Different claim responses will assist in managing the outcome of the claim eg. if the claim status is "To be send" the claim still needs to be submitted.
Ensure payments are processed
When a medical aid received and processed the claim, and everything has been accepted the hospital will receive the money in the next payment run depending on the medical aid.
Most medical aids will send an ERA (Electronic remittance advice) with email or when you use GoodX ERA's you will receive the payment advice in GoodX as an ERA.
ERAs save a lot of time and leave less room for human error in the capturing and allocation process of payments received from medical aids. Manual interventions are few and the time saved with the ERAs can be better used to do debt management or other
necessary tasks.
Wait to allocated and post payments with ERA until the payment from the medical aid show on the hospital's bank statement.
Resolve Claims
- Claims that have been accepted by the medical aids and the payment has been received, can be marked as resolved.
- To resolve claims will assist in knowing which claims still needs work on and which must be followed up with the medical aids.
- Claims that have been accepted but marked that they will not be paid, should also be resolved and the debt should be marked as patient liable.
Print and email the final account
The final account will show all that was invoiced, the receipts (patient / medical aid), credit notes and journals. The final account will indicate what is still outstanding on the patient and medical aid side.