Best Practice Guidelines: Telehealth Practice Management
Copyright © 2020 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
7. Post-consultation phase
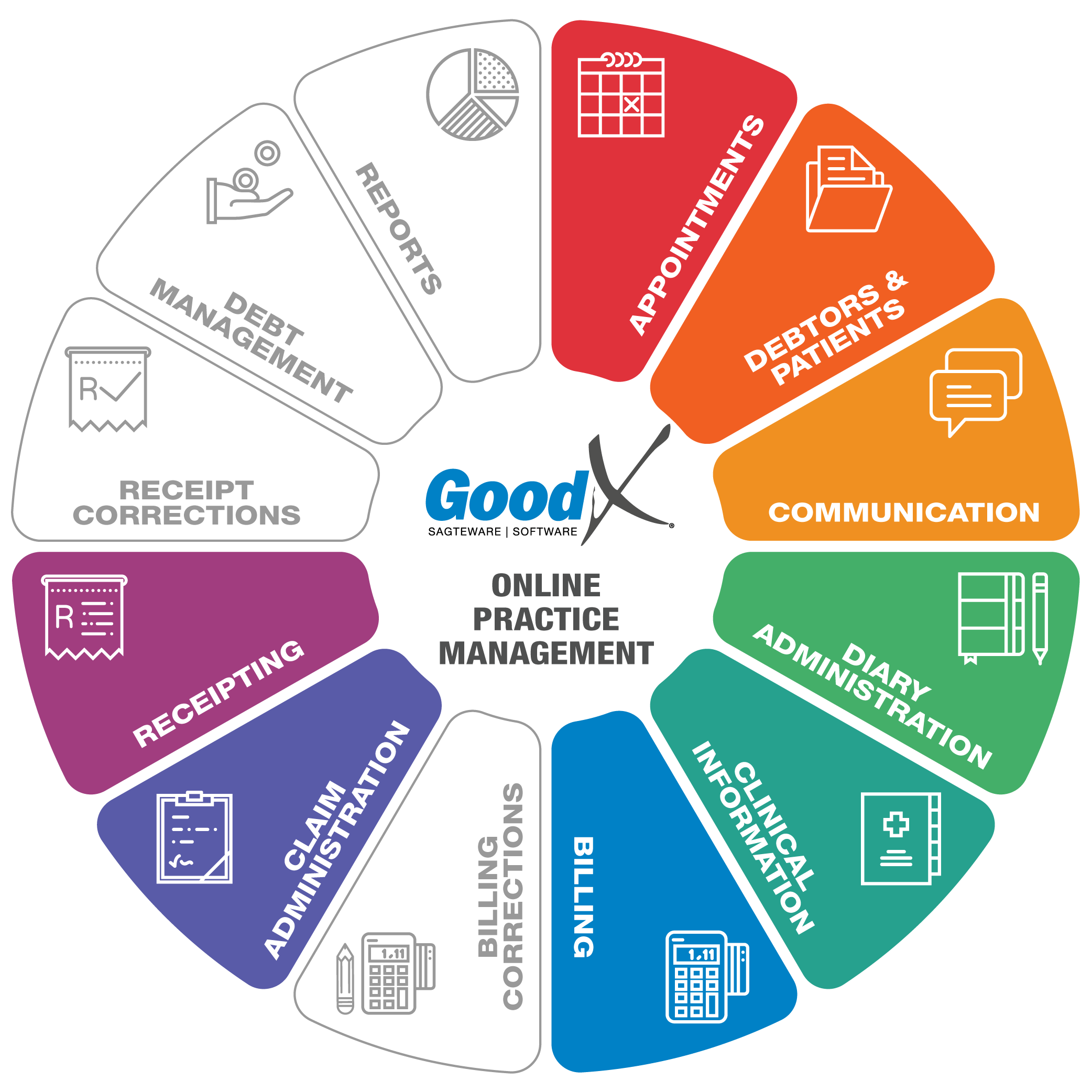
7.2. Claim Administration
Responsible Roles
 |
Validations and Imported data are important tools to prevent rejections. Ensure all claims are sent on a daily basis. Follow up on all rejected claims or line items on the claims immediately, do corrections and resend claims to medical aids. (Complete the 4 R’s: Reverse, Redo, Resend, Resolve.) Ensure all claims are dealt with and that Approved-in-full claims are resolved to update the list which the Credit Controller uses to follow up on outstanding claims. |
|---|---|
|
|
Ensure all possible methods are used to correct claims and all claims are sent to medical aids. Ensure medical aids receive all claims so that payment can be received with the next payment run of the medical aids. Ensure correct claims
are marked as resolved and that claims that have not yet been resolved, are flagged for debt collection. |
 Purpose of Claim Administration
Purpose of Claim Administration
- Claim administration includes private patient accounts and medical aid patient accounts.
- Cash flow is of vital importance to the health of a practice. One way of optimising the cash flow is to send your claim through to the medical aid before the patient leaves the practice so that the cashier will know if the medical aid will settle
the account in full.
- Claim administration assists the practice to keep outstanding debt to the minimum.
- If the claim is rejected by the medical aid, the cashier can inform the patient immediately and receive payment directly from the patient before he or she leaves the practice.
- Claim administration assists the Practice so that Debt Management runs smoothly.
- We are referring to the 4 R’s - Reverse, Redo, Resend, Resolve.
- Claim Administration is an ongoing process until the claim is resolved. The following diagram is the process flow that each claim must follow:

Tasks associated with Telehealth Claim Administration
After creating an invoice for the patient, the claim needs to be submitted, either to the patient’s medical aid or directly to the private patient.
Medical aid procedure summary:
You should check the response from the medical aid, preferably immediately after the claim was submitted, as most medical aids will respond immediately.
The Claim will either be:
- Approved. Remember that this is only an indication and not a guarantee for payment - anything can still happen from the time the claim was submitted until processing for payment. OR
- Rejected for reasons of faulty information (which should be limited if validations were done) OR
- Approved but short paid.
Follow up on rejections and resolve all issues on the rejected claims, for example, if the patient or medical aid details were incorrect. Such issues on claims must be rectified daily.
Resubmit the claim after errors were resolved.
If the claim was rejected due to insufficient funds, an Invoice can be emailed to the patient to ensure immediate payment, and a payment request should be sent.
When the medical aid denies receipt of the claim, proof of submission with the transmission number can be sent through the system to the medical aid.
Private patient procedure summary:
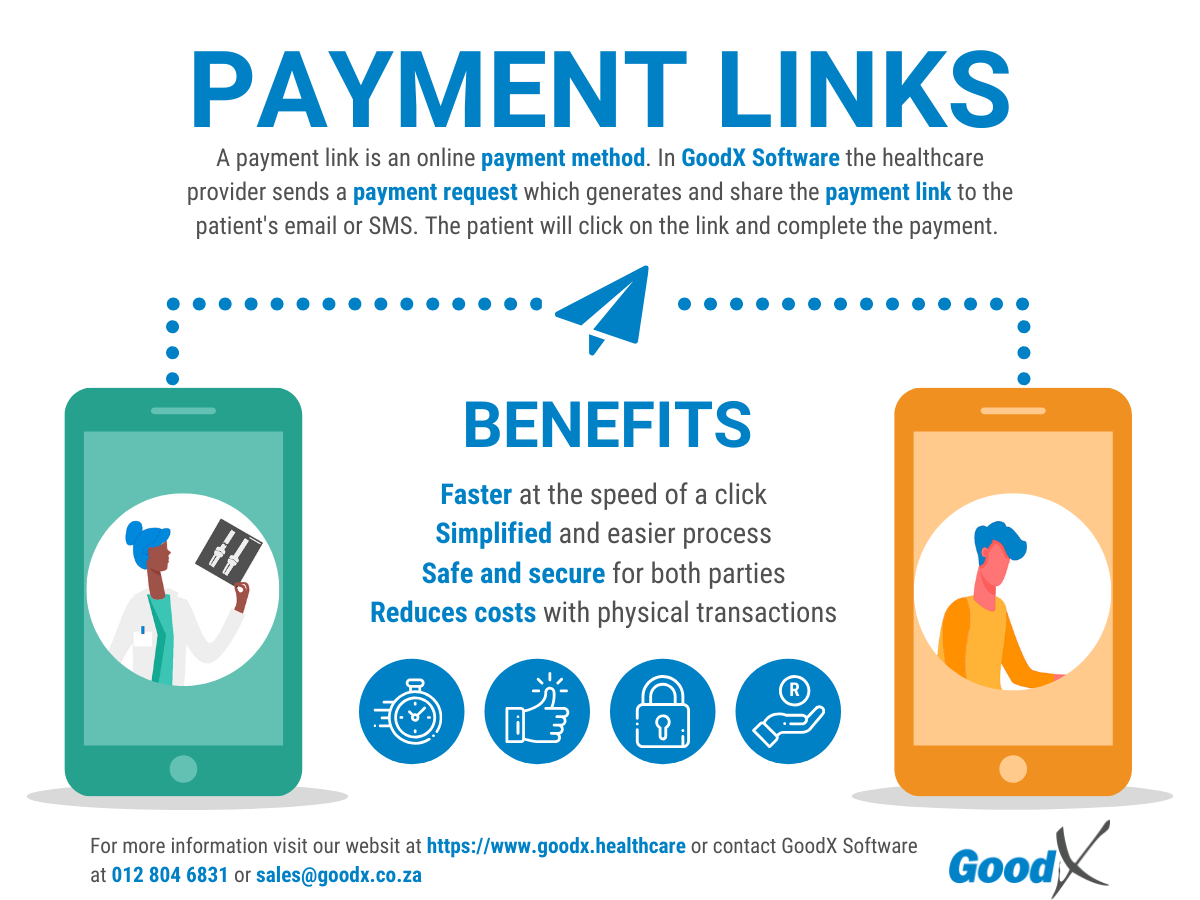
An Email or SMS with a Payment link can be sent to the patient if the patient is a private patient, a patient whose benefits have been depleted or a patient who’s medical aid only paid partially for the claim.
Check if the communication was sent successfully and follow up on all payment links to see if they were paid.
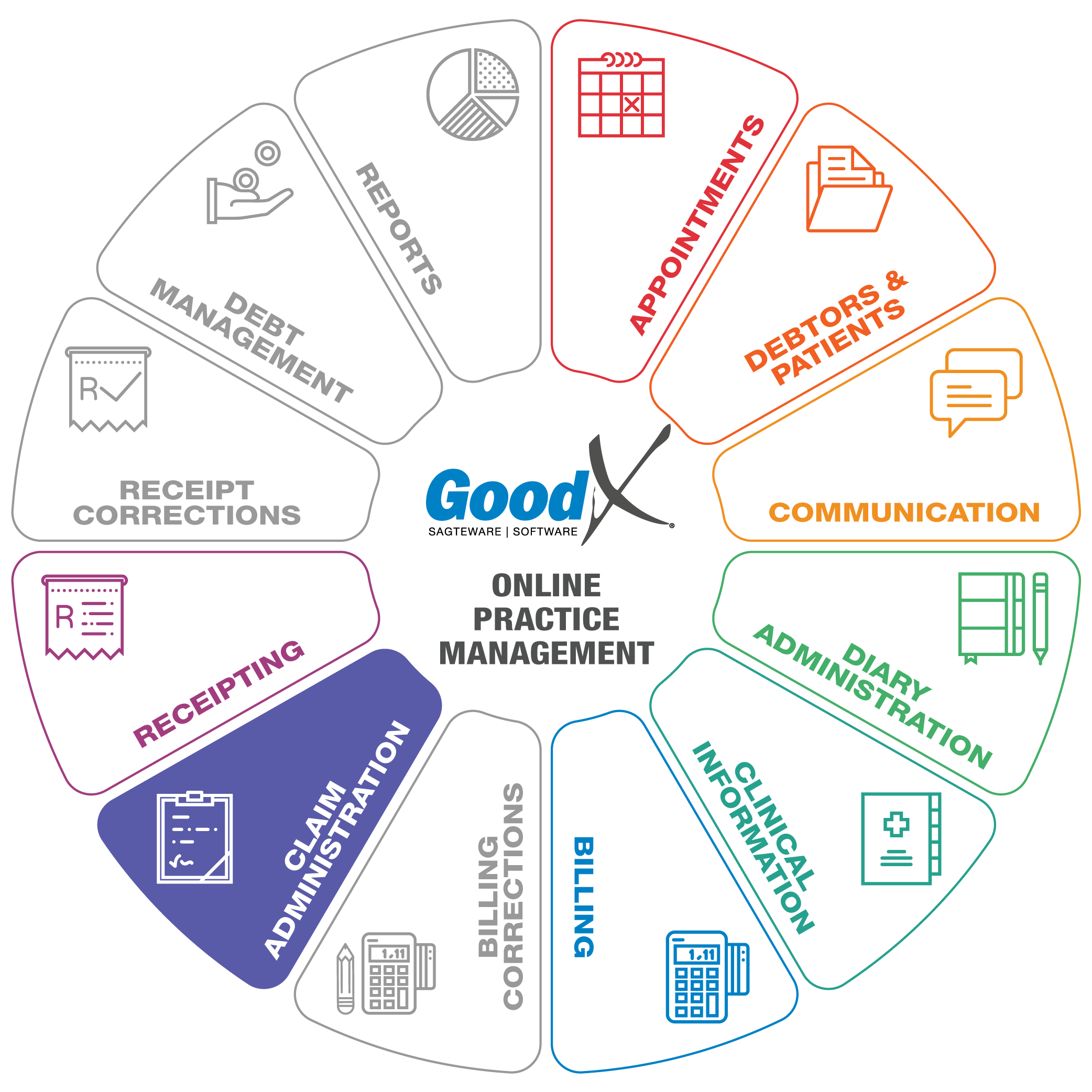
Telehealth claim administration will consist of the following 3 options:
- Private Patient (High financial risk) - Payment link should be sent
- Medical Aid (Low financial risk) - Submission to the medical aid
- Medical Aid Rejection or Shortfall (High financial risk) - Payment link should be sent
Types of Claims:
In this table, you can see the difference between high financial risk claims and low financial risk claims.
 |
 |
|---|
Ensure the following is in place to ensure minimal financial loss:
Private Patient and Medical Aid Depleted (Deposit/Payment link):
Private patients and medical aid patients whose benefits are depleted should preferably pay deposits before having the Telehealth consultation.
In a physical location, it is easier to get the patient to make a deposit at reception, or to stop the patient after the consultation to get payment of the invoice for the consultation. If a patient has received a Telehealth consultation without the deposit, you will only be able to send them their invoice with a payment request and hope they settle the outstanding amount.
Ensure the deposit has been received and allocated to the patient's account. Online payment links can also be used to let the patient pay the consultation. Ensure the SMS/email history is checked daily, to ensure the payment links have been sent successfully to the patient.
Medical Aid Rejections or Shortfall (Payment link):
A payment link should be sent to the patient immediately, to pay the shortfall or any codes that were rejected from the medical aid.
The following information is important with any Claim Administration:
Import Data directly from medical aids
- Import data from medical aids is an important step in any claim administration. This ensures the correct demographic information as it is coming straight from the medical aid of the patient.
- The information will differ from medical aid to medical aid, depending on the information that the medical aid shares with the system.
Validation against medical aid data
- Validations can be used whenever a patient requests a booking, to ensure the information on the system is still correct and that the membership is still valid and active on the medical aid.
- All information must be correct to ensure the claim will go through to the medical aid, with the correct demographic information for both the patient and the main member.
Benefit Check
- Assists in checking if there are available funds for the claim that must be processed. The Practice can do up to 3 benefit checks on a patient per day. The system allows the practitioner, billing expert or receptionist to check for a certain amount. The system will indicate if the required amount is available or not.
- Please take note that this is only an indication, and any other practice can submit their claims. The medical aid will then process that claim first, so your practice’s claim can still be rejected for insufficient funds.
- Important rule: Submit the claims as soon as the patient is done with consultation/treatment to ensure the correct outcome.
Real-time submission through GoodX Switch
- After the consultation, and preferably before the patient leaves the Telehealth video consultation, the claim needs to be submitted to the relevant medical aid.
- An immediate response from the medical aid would indicate if the claim was processed successfully or with a short payment. The patient should then settle the short payment before leaving the Telehealth consultation.
- Most of the medical aids have a real-time submission, but some smaller medical aids will only indicate that the claim was received, and not if the medical aid is going to pay the claim in full or not.
- Always follow up on all medical aid claims. A claim that was 100% processed successfully and accepted by the medical aid, full payment is not guaranteed until the money reflects in the practice’s bank account.
Manage claims
- View responses from the medical aid daily, preferably immediately after the claim was submitted to prevent stale or rejected claims not getting resolved.
- Follow up on rejections and resolve issues on the rejected claims, for example, if the patient or medical aid details were incorrect. These issues must be rectified daily. Resubmit the claims after it was resolved.
- If the claim was rejected due to insufficient funds, an Invoice can be e-mailed to the patient to ensure immediate payment, and a payment request should be sent.
- Different claim responses will assist you in managing the outcome of the claim for example if the claim status is "To Send" the claim still needs to be submitted.
- The rejected claims must be corrected and resend daily, and not left stale and unresolved.
- Ensure all rejected or unsent claim responses have been resolved.
- When a medical aid says that the claim was not received a proof of submission with the transmission number can be sent through the system to the medical aid.
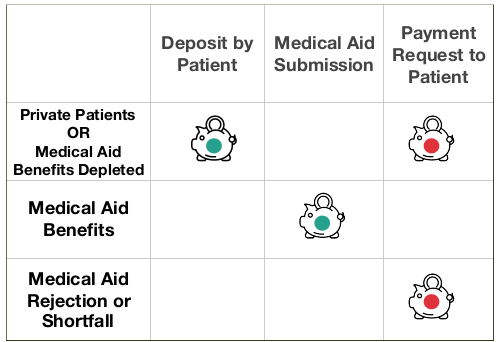
Payment links
- All payment links should be followed up.
- Ensure all payment links went out to the patients successfully.
- Ensure the patient's details are correct and the patient did receive the payment link and understand how the payment links work.
- Ensure to check the SMS/E-mail history daily.
Claim Response
- The claim response will indicate if the claim was processed with or without any rejections and whether the claim will be paid in full by the medical aid.
- The claim response must be checked on every claim after it has been submitted to prevent non-payment and rejections.
- The response will also show the line items that were rejected, with a reason why the line item will not be paid. This can be corrected and the claim can be resubmitted.
- This is only an indication and not a guaranteed payment - anything can still happen from the time the claim was submitted to the medical aid processing it for payment.
If any mistakes were made on a Claim, you can amend the mistake by doing a Reversal of the claim, Redo the Invoice and Resubmit it.
Ensure the correct steps are taken to ensure the correct information is sent to the medical aid and no duplicate claims errors are received.
Claim History Screen
- The claim history screen is the most important in the Claim Administration process.
- Claim history has all the information about when the claim was sent to the medical aid, the response from the medical aid, rejections and reversals.
- The Claim history screen must be checked daily to follow up and resolve the claims that were submitted to the medical aid.
- Some of the Functions on the Claim History screen is as follow:
- Send claim
- Reverse claim
- Response
- Patient Validation
- Resolve claim
- Move outstanding amount to Patient or Medical Aid
- SMS and Viewing the account
- The Claim History screen is also a worklist to resolve all the claims and to ensure that the claims do not go stale.
Resolve claims
- To resolve a claim is to mark the claim resolved. This will indicate that the claim has been sorted out and every possible solution was done on the claim to ensure payment or that the payment was received from the medical aid.
- Claims can be marked resolved if:
- They have been accepted by the medical aid
- They have been accepted but marked that they will not be paid. The claim should be moved to the patient liable.
- They were paid in full.
- The claim history screen should not be used for collection purposes. The credit-control assistant was specifically designed to assist practices in following up on outstanding debt.
- The process must be agreed on by the practice when a claim will be marked as resolved:
- when the claim is fully processed and all rejections were dealt with or
- when the payment was received from the medical aid
- Remember that there are Debt collecting processes in the system to ensure that the debt management process runs smoothly.
- The main focus is to have only the claims that need to be followed up on as unresolved claims. This allows the credit controller to focus only on the unresolved claims and try to resolve it with the medical aid.
- Important functions that will be used to ensure correct claim administration
