Best Practice Guidelines: Healthcare Practice Management & POPIA Compliance Framework
Best Practice Guidelines: Healthcare Practice Management
&
POPIA Compliance Framework
Copyright © 2021 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
8. Clinical Information: Roles & Purpose
8.6. Treatment Plan
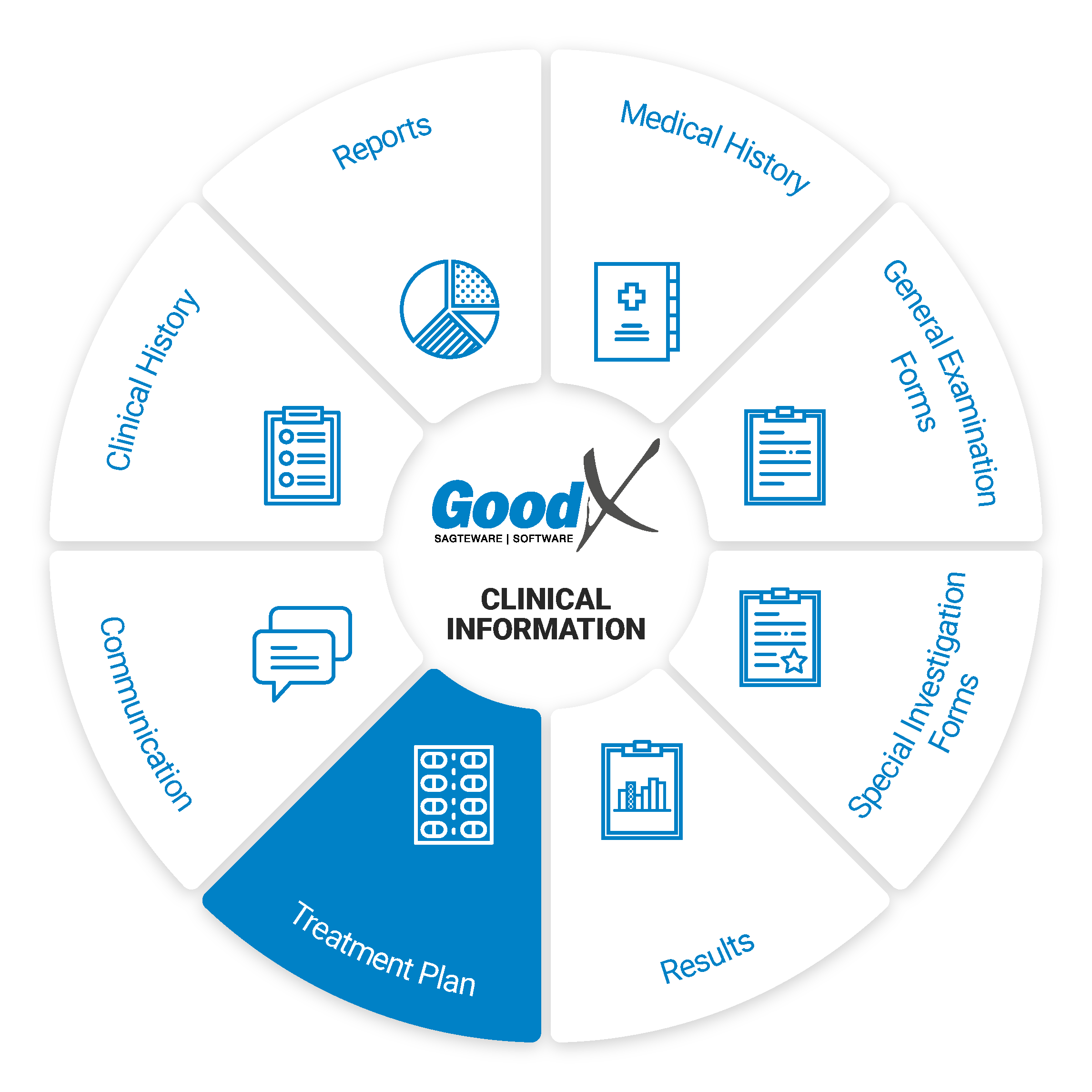 A treatment plan contains
details about the patient’s condition as well as the practitioner’s recommended treatment. Anything that the practitioner uses to assist n making the patient condition better can be recorded/documented in the treatment clinical forms. Following will be an explanation of some of the clinical forms that the practitioner can use to assist them with the treatment of the patient:
A treatment plan contains
details about the patient’s condition as well as the practitioner’s recommended treatment. Anything that the practitioner uses to assist n making the patient condition better can be recorded/documented in the treatment clinical forms. Following will be an explanation of some of the clinical forms that the practitioner can use to assist them with the treatment of the patient:
Authorisation Setup
For certain procedures or treatments, the patient will need authorisation from their medical aid to proceed with the treatment or procedure. The Practice can provide the patient with an Estimate (quotation) for the procedure with the ICD-10 codes, procedure codes and costs. The patient can then send this to their medical aid to obtain an accurate authorisation of what will be covered and what not.
The authorisation number received from the patient medical aid will be an indicator that the medical aid will pay for the procedure or treatment that they’ve agreed on. An authorisation will also have a start date and end date, with an amount that was approved.
When the Authorisation number has been received the authorisation can be set up on the patient electronic file to pull through to the billing and go through to the medical aid when the invoice is switched.
The authorisation number must be included in the billing to ensure payment from the medical aid.
Scripts/E-Scripting or Prescription Letter
Scripts will allow the patient to get the necessary medication to aid in his/her treatment from any pharmacy. The script form has a lot of features that make scripting a quick and easy process, the practitioner can decide which features suit their workflow. When the script is printed or emailed from the system, signed electronically by the Practitioner, a watermark 'NOT ORIGINAL' will display on the script.
The system can create scripts (Can be used as a hardcopy) as well as e-scripting. Though e-scripting is not new technology, the many features of e-scripting in GoodX Software are rapidly evolving into a tool that significantly benefits healthcare practitioners, patients and pharmacists.
Core features of scripts to capture and exchange information:
GP to Pharmacy to GP
Practitioners can push scripts to selected pharmacies and mark the medications as non-substitutable, ensuring that only the originally prescribed product is dispensed. Data is pushed back to the practitioner for recordkeeping and adherence information as soon as the medication is dispensed. In other words, you as a doctor can see what and how much medicine was dispensed to your patient.
Electronic Medical Records (EMR)
As soon as the practitioner captures clinical information into the software solution, the information becomes part of the electronic clinical history of the patient. All future treatment plans will then automatically be informed and guided by the patient’s clinical history.
When, for example, chronic scripts have to be refilled, the software will provide a list of issued scripts from which the practitioner can choose, eliminating the unnecessary time spent to research the history of the chronic medication. In addition, an inline scripting history adds the list of chronic medication lines with one button into the current script. Thus, a 20-line script can be refilled in less than 15 seconds, saving the practitioner an immense amount of time.
Acute scripts
The most basic script that can be created is an acute script. An acute script consists of a list of short term medications with directions of use and a diagnosis.
Chronic scripts
Chronic scripts are scripts that contain chronic items. An item can be marked as chronic by either manually marking the item as chronic or by marking the item as more than five times repeatable. When a script as a whole is marked as more than five times repeatable all of the script items will be marked as chronic.
Directions builder
Every script line has a directions builder which assists the practitioner in creating directions of use for each script item. The directions builder allows the practitioner to populate the directions field by selecting options from some dropdowns (for example, time of day, meal relationship and route) and entering numbers in some fields (for example, dosage, frequency and days supplied).
The signata can be set up with a shortcut and a description. GoodX has a default list that can be used. This is a preset list of directions of use.
Example: When "1B14" is typed in the following will display in the signata column: TAKE ONE IN THE MORNING AND ONE AT 14:00.
Script favourites and macros
When creating a script the practitioner can save a script item with its directions of use as a favourite or save a couple of script items as a macro. When creating a script the practitioner can easily add script items by adding favourites/macros to the script.
Script history
The practitioner can quickly recreate any formerly scripted script line or script from the patient’s script history which is displayed at the bottom of the script.
Import chronic lines
Another way to quickly create script lines is to import script lines from the medical history where you can set up a script per chronic condition for each patient.
Generics
On every script line, the practitioner can quickly view generics for the selected script item and easily replace the script item with a generic.
Consumables
Consumables can be included in the script.
Allergy Warning System and Drug Interaction Checker (DIC)
Allergies that are captured and linked to drug classes and active ingredients will trigger the warning system in the software.
While a script is being created the drug interaction checker checks for interactions between all of the scripted items and warns the practitioner about interactions. The practitioner can also open the DIC on the script to see more information about the interactions as well as to see information about the side effects of the medication and the directions of use for each medication.
The drug interaction checker built into GoodX will automatically assess the information on the newly created script and warn the practitioner of any interactions between the medications captured in the script. This feature allows the practitioner to ensure that no interactions will adversely affect the patient and warn the practitioner in advance so that appropriate alternatives can be prescribed.
A holistic view of the patient and all their chronic conditions and allergies is possible through this single platform approach.EM Guidance
Essential Medical Guidance, or EM Guidance, is the leading medicines information platform that exclusively supports medical professionals to accurately and safely prescribe in South Africa and across the developing world.
EM Guidance is a free and trusted online medicines and guideline resource for medical professionals that provides up-to-date information. This product has been integrated into GoodX Software, making crucial medicine information immediately accessible to the practitioner. This feature allows the practitioner to prescribe better for better outcomes due to this expanded knowledge base at the practitioner’s fingertips.
To give a feel for its use, EM Guidance includes the following types of information:
- Medicines: South Africa’s most comprehensive, evidence-based medicines resource.
- Guidelines: Over 1,200 locally relevant clinical guidelines.
- Tools: Growing library of clinical decision support tools.
- Care Coord: Hospital-level information, including call rosters, guidelines and formularies.
The platform is created in partnership with a national network of pharmacologists, specialists and medical academic institutions, so you can trust that the clinical guidelines and medicines information is accurate.
A quick scenario: you’re creating a prescription for your patient via the GoodX Web App and, with a click of a button, easily check the dose, contraindication or interactions between the different prescribed medications via EM Guidance.
The GoodX Software and EMGuidance integration will provide healthcare professionals with intelligent software and reliable medicine and clinical information and ensure that patients receive the best care possible.
Add script lines to the invoice
When the practitioner is done with the script they can add the script lines to the invoice.
Health Window Integration - Medicine Adherence
GoodX Software, through collaboration with Health Window, aims to provide more information by displaying the average adherence rates per product on the scripting platform.
Hovering over the indicator for each drug will show the average adherence for that molecule and whether the product has funding for call centre interventions or digital interventions. Alternative products will be displayed, with the option to switch to one with better adherence rates. Having more patients managed by Health Window will increase patient volumes in the practice. Furthermore, being better informed can result in better clinical decision making and, ultimately, improved outcomes. By choosing products that have invested in adherence, you are giving your patients the best chance of staying on therapy and achieving improved disease control.
In addition to this, Health Window will be monitoring the practice’s patients within their pharmacy network for script expiry and, through integration with the GoodX online calendar, make bookings for patients on the practice’s diary for check-ups and script renewals. This will increase the number of patients returning to the practice.
Continuation of this service depends on Health Window’s access to the dispensing behaviour of patients. When a patient hand in their script at a Health Window affiliated pharmacy, Health Window can track and manage their adherence monthly and direct them back to the practice when the repeat script is due. However, should a patient move out of Health Window’s pharmacy network, this will not be possible, thereby increasing the likelihood of non-adherence and disappearance from your practice.
Electronic signature
The practitioner can sign the script electronically or import their signature from the settings onto the script by using the pin that they set up in the settings along with the signature.
Chronic script reports
A chronic script reporting tool allows the doctor to see which patients are due for renewal and which patients are taking their medicines (provided they fill their prescriptions at participating pharmacies). The doctor can search on the active ingredient, patient or script age.
Manual Override
Manual Override on a prescription allows the user to create a prescription manually without using stock items loaded onto the system. The user will type out their desired items into fields that are provided. Some practitioners prefer to rather do a manual prescription rather than use the items from the stocklist. It will not be possible to use this feature at a practice that keeps and manages stock. Disclaimer: Please be advised that using the Manual Override feature is not encouraged as Medical Adherence, Reports and other integrations will not be available at all. It is suggested to rather use regular scripting as much as possible, where items can be selected from the loaded Medprax or IQuest lists.
Unified platform for dispensing GPs
Dispensing GPs can rest assured that only one software system must be used and maintained for all clinical work and dispensing. Additionally, being able to bill, switch, dispense, print labels and capture electronic remittance advice (ERAs) in one system offers the practitioner the ability to manage his practice and finances effectively.
Repeatable Script
The script can be marked as a Repeatable Script to indicate that the script needs to be repeated, this is usually for chronic medication scripts and long-term use scripts. When the patient comes back the script can be used again without the need to capture everything over again.
Re-print Original
The reprint allows the Practioner to reprint the original script, a watermark will appear to advise that it is a copy of the original when printed. Reprinting a script will allow the user to print a copy of a prescription that has already been created on the system. Scripts are usually reprinted to keep a copy in the patient's hardcopy file as a reference to what was prescribed should the electronic copy not be available, or if a patient has misplaced their copy before they have handed it in at the pharmacy.
The benefits e-scripts offer healthcare providers and patients
Medical practitioners benefit from e-scripts in the following ways:
- The software provides complete insight into the previous prescriptions given to the patient at the click of a button;
- The practitioner will be able to see which medication the pharmacy actually dispensed;
- Allergy alerts and potential drug interactions allow the practitioner to choose medication wisely; avoiding clinical and legal risks;
- The practitioner builds a standard list of medications;
- The practitioner can easily choose generic medicines from the list that Medical Funders cover and, in that way, be sensitive to patient’s financial constraints;
- Fast repeats of previous scripts save time and effort;
- The practitioner can create templates and macros for scripts, enhancing their workflow;
- The paperless workflow saves costs and filing space;
- Medication adherence can be measured and is therefore reportable for future healthcare decisions.
Pharmacists benefit from e-scripts in the following ways:
- e-Scripts received from a trusted software provider using a secured transmission source eliminate the risk of scripting fraud and double dispensing.
- The pharmacist saves time and frustration by avoiding phone calls to practitioners due to illegible handwriting;
- Imported patient and script information saves capturing time and the possibility of human error.
Patients benefit from e-scripts in the following ways:
- Firstly, the patient can easily choose the pharmacy’s location and won’t have to stand in long queues if the pharmacy pre-packed and prepped the medication. It is far better for the prescription to wait for the patient than for the patient to wait for the prescription!
- When e-Scripts are sent directly to the preferred pharmacy, patients won’t lose their scripts, bringing added security to the process and lightening the burden of the patient and the workload of the practice since extra printing is avoided.
- There will be increased chronic medication adherence since the patient will experience a more convenient way of acquiring their medication.
- Patients can have a more meaningful conversation with their pharmacist if they do not have to pick and pack the medication. Instead, patients won’t feel the pressure of a long queue waiting for them if they would like to discuss their medicines with their pharmacist.
- When the practitioner sends the medication to the pharmacy, the patient information accompanies the e-script, saving capturing time and reducing human error. In addition, by the time the patient arrives at the pharmacy, their information is already in the pharmacy system, making the engagement at the pharmacy highly convenient.
The e-scripting in GoodX Software makes it very valuable to practitioners, patients and pharmacists. So, if you are still using any other means of scripting, it is time to reconsider the benefits of e-scripting.
Print Medicine/Signata Labels
Signata Label is the label that indicates how the medicine must be taken or used. The Signata Label is the directions on how to use the medicine. The label can be stuck on the box or bottle with the patient information and expiry date of the medication.DAMA
Dama: Disease Administration and Management Assistant
The purpose of the DAMA Protocols in GoodX: In a healthcare setting, a protocol, also called a medical guideline, is a set of instructions that describe a process to be followed to investigate a particular set of findings in a patient or the method which should be followed to control a certain disease. In short, this is a Treatment Plan that will inform the Patient when to do certain tasks with regard to his/her condition.
Practitioners will be able to set up protocols for their Patients through DAMA. This will help them to monitor their patient's condition and also remind the patients to take their medicine etc on a regular basis for example.