Best Practice Guidelines: Healthcare Practice Management & POPIA Compliance Framework
Best Practice Guidelines: Healthcare Practice Management
&
POPIA Compliance Framework
Copyright © 2021 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
8. Clinical Information: Roles & Purpose
8.3. General Examination Forms
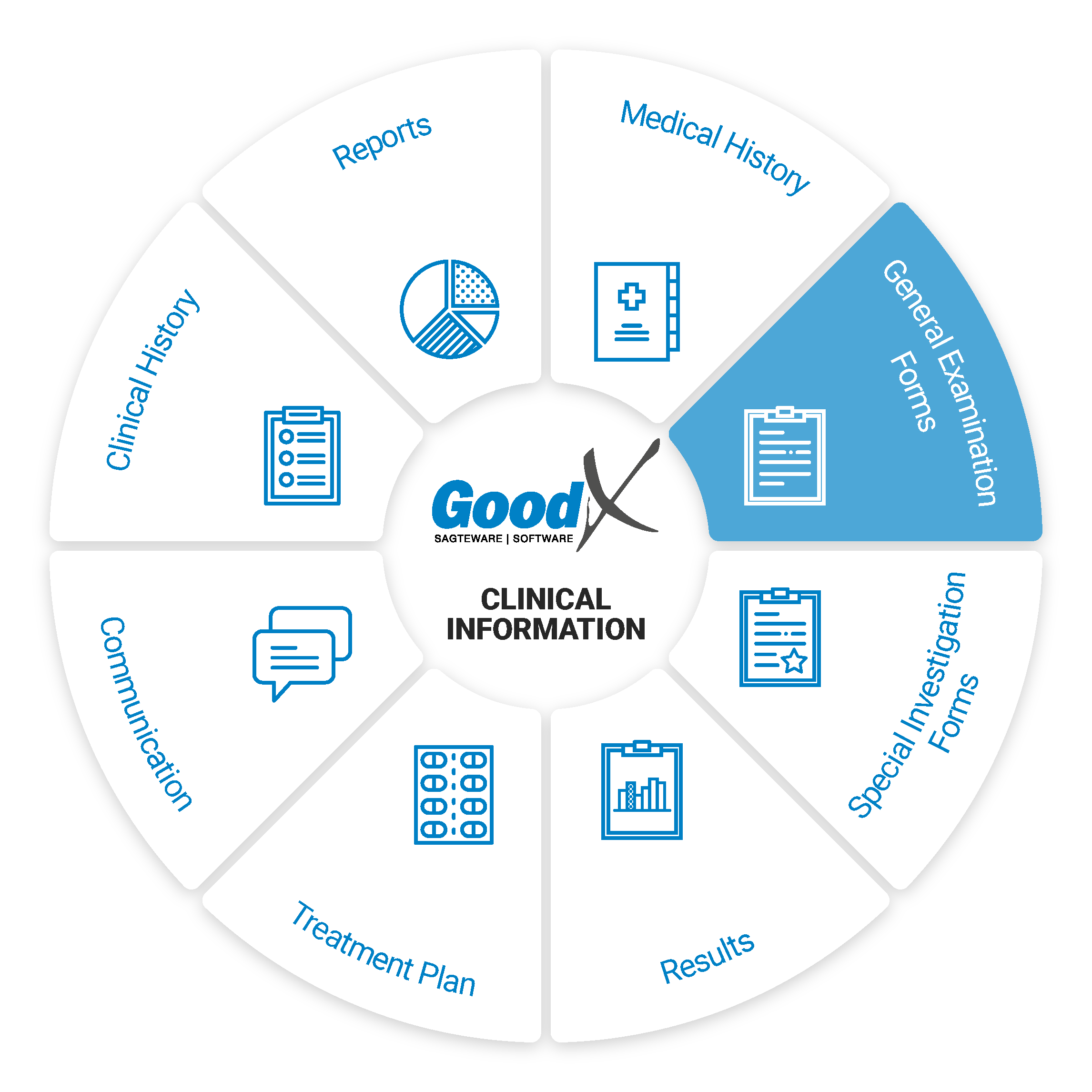
General Examination Forms
The general examination forms are used to record observations made during a patient examination. Here we’ll discuss some of the general examination forms that can be used on a daily basis:
- General Examination
- Quick Note
- Triage Form (Triage/ER Practices)
- Different WCA Forms
- Covid Questionnaires
General Examination (GPE)
This form is structured in such a way to help practitioners quickly and easily capture their observations. The values entered into this form will also become part of the patient’s clinical history which can be reviewed to see whether a patient’s health has improved/declined over a period of time. When abnormal measurements are entered it will be indicated in red on the form. This form includes the following sections:
Physical Examination
In the Physical Examination, the Practitioner will listen to the patients and capture all the information of the condition and complaints.
Medical History
Medical History is a record of health information about a patient and his or her close relatives that should be recorded by the Medical Practitioner and will affect the way that the patient is diagnosed and treated. The Medical History in the Physical Examination will pull through the information from the Medical History captured on the patient file, for example, the:
- Allergies
- General History
- Vaccinations
For more information on the Medical History, please refer to the Medical History Sub Chapter in the Clinical Information section.
The Physical Examination is used to capture the following details:
- Complaint - What the patient says is the problem.
- Notes - Any notes the practitioner needs to remember about the patient condition and general examination.
- Images - Any images can be uploaded onto the general examination, for example, the patient has an injury and the practitioner needs to keep track of how the wound progress with the follow-up consultations.
- Symptoms - The practitioner needs to capture all the symptoms the patient have or complain about.
- History - Allergies, General History (General Health and Family History) and Vaccinations the patient has or did receive in the past.
- Vital measurements - for example, blood pressure, pulse rate, temperature, BMI, waist/hip ratio or FRAMINGHAM score.
- Sideroom investigations - for example, urine test, glucose, cholesterol, HIV, malaria, HDL.
- JACCOLD - Jaundice, Anaemia, Clubbing and Spooning, Cyanosis, Oedema, Lymphadenopathy and Dehydration.
Review of Systems
In the Review of Systems section, you will find system visualisations, space to make notes about each sub-system and in some subsections, you will find quick capture features like yes/no questions that allow the practitioner to easily capture their findings. The practitioner can also make annotations on the system visualisations. The information in this section can assist the practitioner in planning the treatment of the patient. This section is split into the following sections (subsections under each section will be indicated by the information between the brackets):
ENT and Ophthalmology
The ENT and Ophthalmology section can be used to capture information about the patient's eyes, ears, nose, mouth, throat, facial views and general notes on the ENT and Opthalmology.
The ENT and Ophthalmology section should be completed when the practitioner examines the patient eyes, ears, nose, mouth, throat, head or neck.
Respiratory
The Respiratory section will be used to capture the patient condition on signs of distress, chest wall, patterns of breathing, palpation, percussion, auscultation.
The human respiratory system is a series of organs responsible for taking in oxygen and expelling carbon dioxide. The primary organs of the respiratory system are the lungs, which carry out this exchange of gases as we breathe.
Cardiovascular
The Cardiovascular section will be used to capture the patient conditions on the patient heart rate, heart sounds/murmurs, precordial palpation, JVP/neck veins, ECG and general notes on the cardiovascular system.
The cardiovascular system comprises the heart and blood vessels and carries nutrients and oxygen to the tissues of the body.
Abdominal
The Abdominal section will be used to capture the patient condition on the inspection, palpation, percussion, auscultation and general notes on the patient abdominal condition.
The abdomen includes a host of organs including the stomach, small intestine, colon, rectum, liver, spleen, pancreas, kidneys, appendix, gallbladder and bladder.
Musculoskeletal
The Musculoskeletal section will be used to capture the patient condition on the patient head, gait, arms, legs, spine and general notes of the musculoskeletal system.
A combination of the muscular and skeletal systems working together includes the bones, muscles, tendons and ligaments of the body.
Genito-urinary
The Genito-urinary section will be used to capture the condition of the patient on the patient breasts, cervix, inspection, palpation, percussion and general notes of the genito-urinary system.
The genito-urinary system or urogenital system is the organ system of the reproductive organs and the urinary system.
Lymphatic
The Lymphatic section will be used to capture the patient condition on Inspection and general notes of the Lymphatic system.
The lymphatic system is part of the vascular system and is an important part of the immune system, comprising a large network of lymphatic vessels that carry a clear fluid called lymph directionally towards the heart.
Immunological/Endocrinology
The Immunological/Endocrinology section will be used to capture general notes of the patient condition.
The immune system is the body's defence against infectious organisms and other invaders and endocrinology is the collection of glands that produce hormones that regulate metabolism, growth and development, tissue function, sexual function, reproduction, sleep, and mood, among other things.
Dermatological
The Dermatological section will be used to capture general notes of the patient condition
Comprises the skin and its appendages acting to protect the body from various kinds of damage, such as loss of water or damages from outside. The integumentary system includes hair, scales, feathers, hooves, and nails.
Psychiatric
The Psychiatric section will be used to capture the patient condition on ADD, ADHD, anxiety, bipolar disorder, depression, OCD, substance dependency and general notes.
A psychological disability or psychiatric disability refers to a spectrum of mental disorders or conditions that influence our emotions, cognitions, and/or behaviours.
Neurology
The Neurology section will be used to capture the patient condition on cranial, dermatomes, reflexes, sensory system, motor system and general notes.
The nervous system is made up of two parts: the central and peripheral nervous system and deals with disorders of the nervous system. It includes the brain, spinal cord and nerves.
Diagnosis & Plan
Diagnosis and Plan assist in planning the patient's treatment and recovery. Assisting in the following:
- Quick once-off diagnosis.
- Easy guided custom procedures.
- Single click invoicing and direct scripting.
- The treatment plan can be built and will assist in knowing what to expect and when important dates for follow-ups are necessary.
Quick Note
The quick note can be used to make short notes and add pictures when a practitioner does not want to use the General Examination form. It can also be used to capture any additional information about the patient examination. The quick note is a free text function, the practitioner can add any information into the section with special features, for example, to bold some of the text, or put in bullets to assist in better reading of the notes that were made.
Covid19 Questionnaire + Screening
- The questionnaire form is a research instrument consisting of a series of questions for the purpose of gathering information from patients regarding their Covid risk level. Questionnaires have advantages over some other types of surveys in that they are cheap, do not require as much effort from the questioner as verbal or telephone surveys, and often have standardised answers that make it simple to compile data.
- The Practitioner will immediately have the response/results on the GoodX system after the Patient completed the Questionnaire that the practice sends to them via SMS or email.
- The Patient will receive an SMS or email once they have booked a Telehealth appointment online, with a LINK that will redirect them to a pre-screening questionnaire that they should complete determining their risk.
- The COVID-19 pre-screening questionnaire will have a drop-down next to each question to complete your answer. Each question will have points allocated to it, this will determine the patient's risk of having the virus which will reflect on the Doctors Diary on the Patients appointment.
Triage Form - Nurses
- A Triage form is a clinical form that the ER nurses use to check the patient's vitals and appearance.
This form automatically changes the colour of importance regarding the information that the nurse completes to determine the risk the patient is at.
![]()
GoodX also has a Triage process that is connected to an EMR Form. Please refer to our Learning Centre for more information on the Triage and available courses on the Triage process.
WCA (Workers Compensation Act) and RMA (Rand Mutual Assurance) for IOD (Injury on Duty) Forms
- The Compensation Fund (WCA) and Rand Mutual Assurance (RMA) are the only two injuries on duty (IOD) funds that can be submitted through the GoodX Switch.
- Workers compensation is a form of insurance providing wage replacement and medical benefits to employees injured in the course of employment in exchange for mandatory relinquishment of the employee's right to sue his or her employer for the tort of negligence. There are four distinct types of Workers compensation benefits:
- Medical treatment benefits.
- Disability benefits.
- Supplemental job displacement benefits.
- Death benefits.
The forms in GoodX Software are split between WCA and RMA forms. There are multiple forms available for the practitioner to complete for both parties.
- Multiple WCA Forms available for the Practitioner to complete:
- WCA Disease First report: The purpose of the Disease first report is for the Practitioner to capture and provide full details on the IOD for the patient and the symptoms the patients are experiencing.
- WCA Disease Progress or Final Report: The purpose of the Disease progress or final Form is for the Practitioner to capture and provide the progress of the Patient after the first report was done.
- WCA Exposure History: The purpose of the Exposure History Form is for the Practitioner to capture and provide information regarding the environment in which the employee has been exposed to His/Her disease.
- WCA Final: The purpose of the WCA final report is for the Practitioner to capture and provide full details on the progress and end results for the patient. The final report will be done after the patient was treated and what the final outcome for the injuries sustained is.
- WCA First Report: The purpose of the WCA first report is for the Practitioner to capture and provide full details on the IOD for the patient. When the injury/accident took place etc.
- WCA Follow Up: The purpose of the WCA follow up report is for the Practitioner to capture and provide full details after the patient was treated and if the patient should come for a follow-up and what the follow-up appointment will include.
- WCA Reopen: The purpose of the WCA Reopen Report is when the patient IOD was finalised in the past but the patient injury or illness have returned after a certain period for the same injury or illness and the patient need treatment again.
- Multiple RMA Forms available for the Practitioner to complete:
- RMA First Report: The RMA - 1 - First Report document must be completed by the practitioner and all the details and related documents must accompany the claim to be confirmed and submitted.
- RMA Progress Report: The RMA - 2 - Progress Report will be completed and submitted after the initial Injury on Duty consultation when the RMA - 1 - First Report was completed and the practitioner came to the conclusion that there is a need for a follow-up consultation. The report will state whether the patient has improved since the first consultation and whether the patient has needed to undergo further tests, surgeries and treatments in order for their condition to become stabilised.
- RMA Final Report: The RMA - 3 - Final Report will be completed and submitted after the initial Injury on Duty consultation when the RMA - 1 - First Report and RMA - 2 -Progress reports have been completed. The practitioner has concluded their findings and everything has been done to ensure that the patient is healthy or that there is nothing further that can be done medically for the patient.