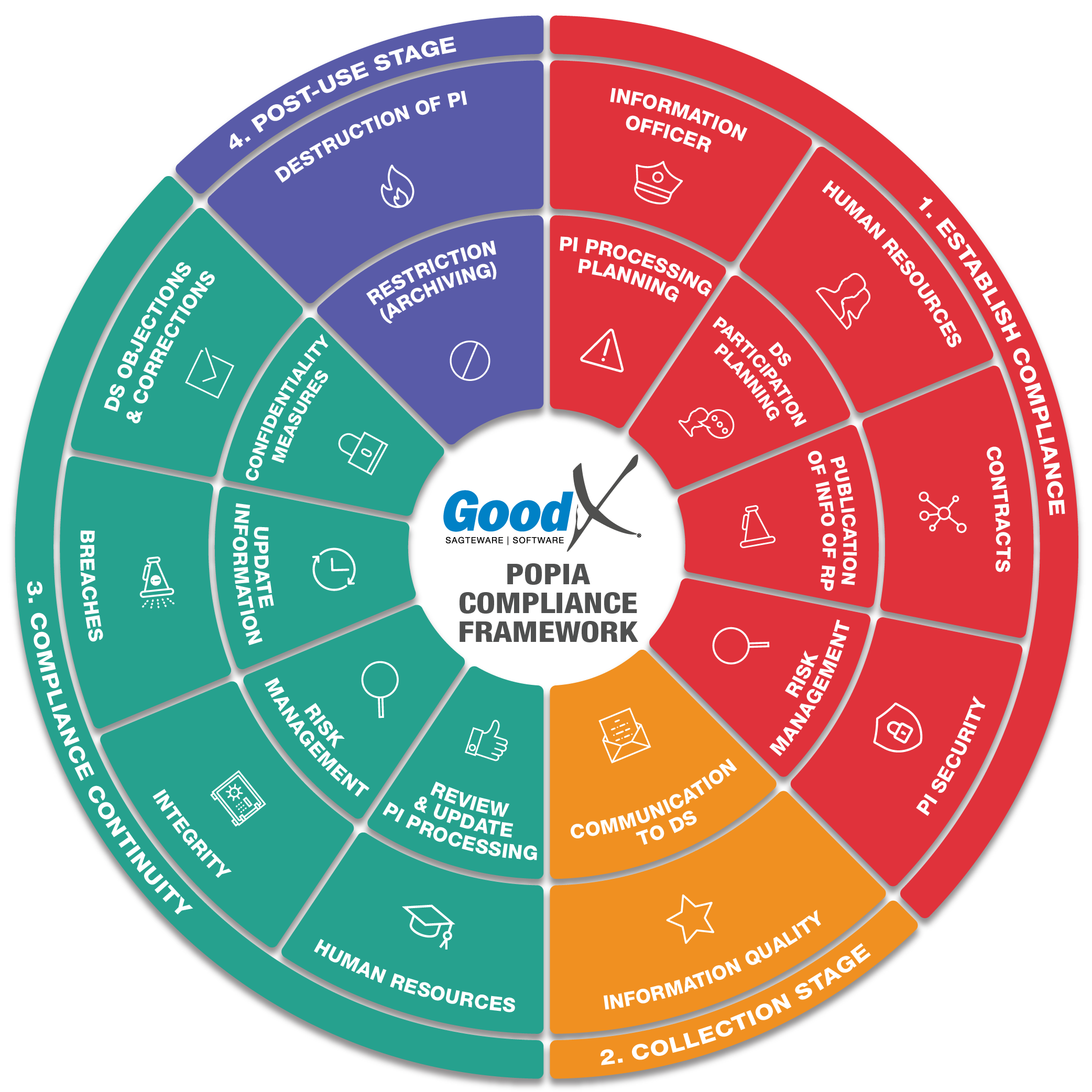
Best Practice Guidelines: Healthcare Practice Management & POPIA Compliance Framework
Best Practice Guidelines: Healthcare Practice Management
&
POPIA Compliance Framework
Copyright © 2021 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
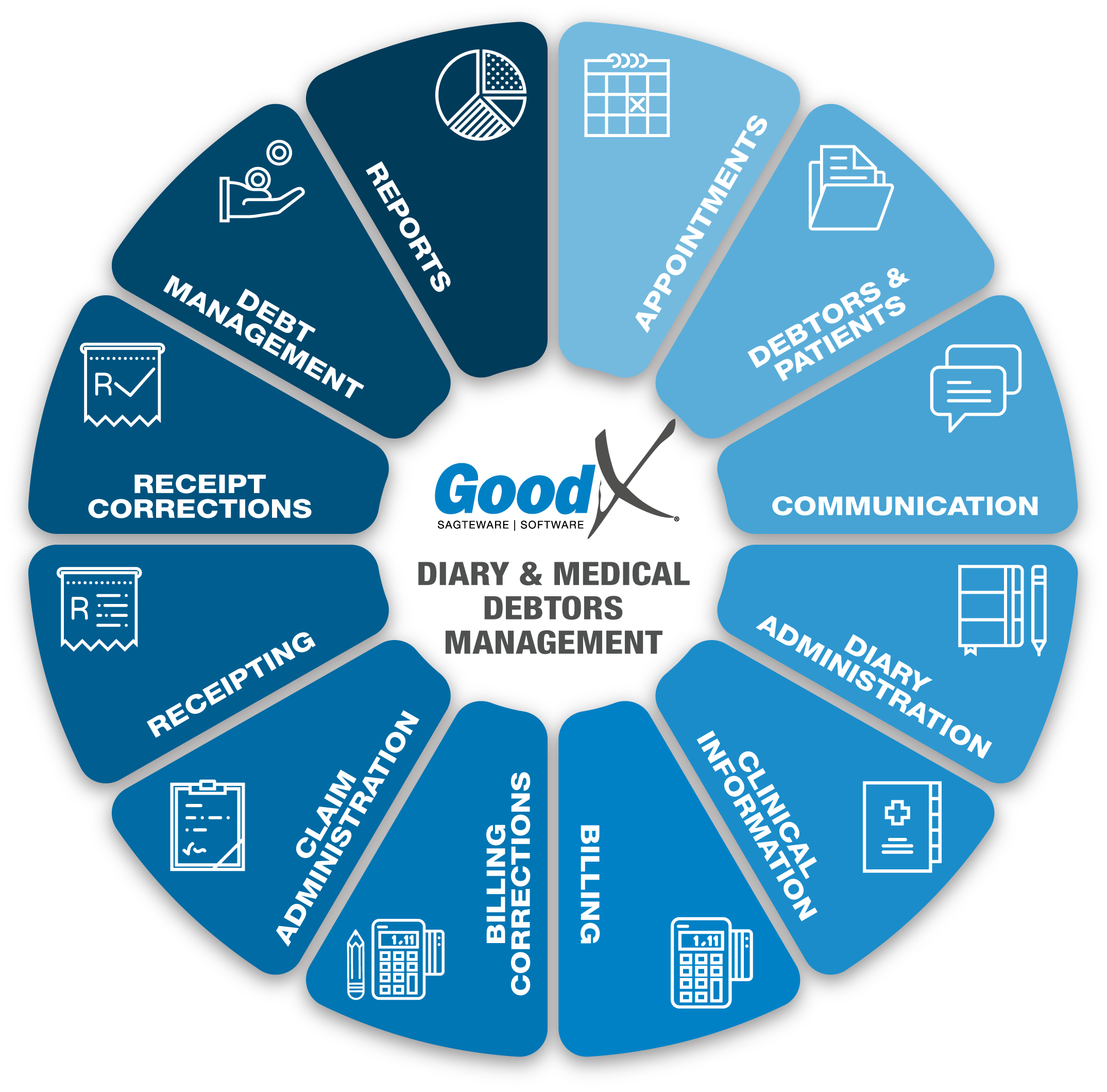
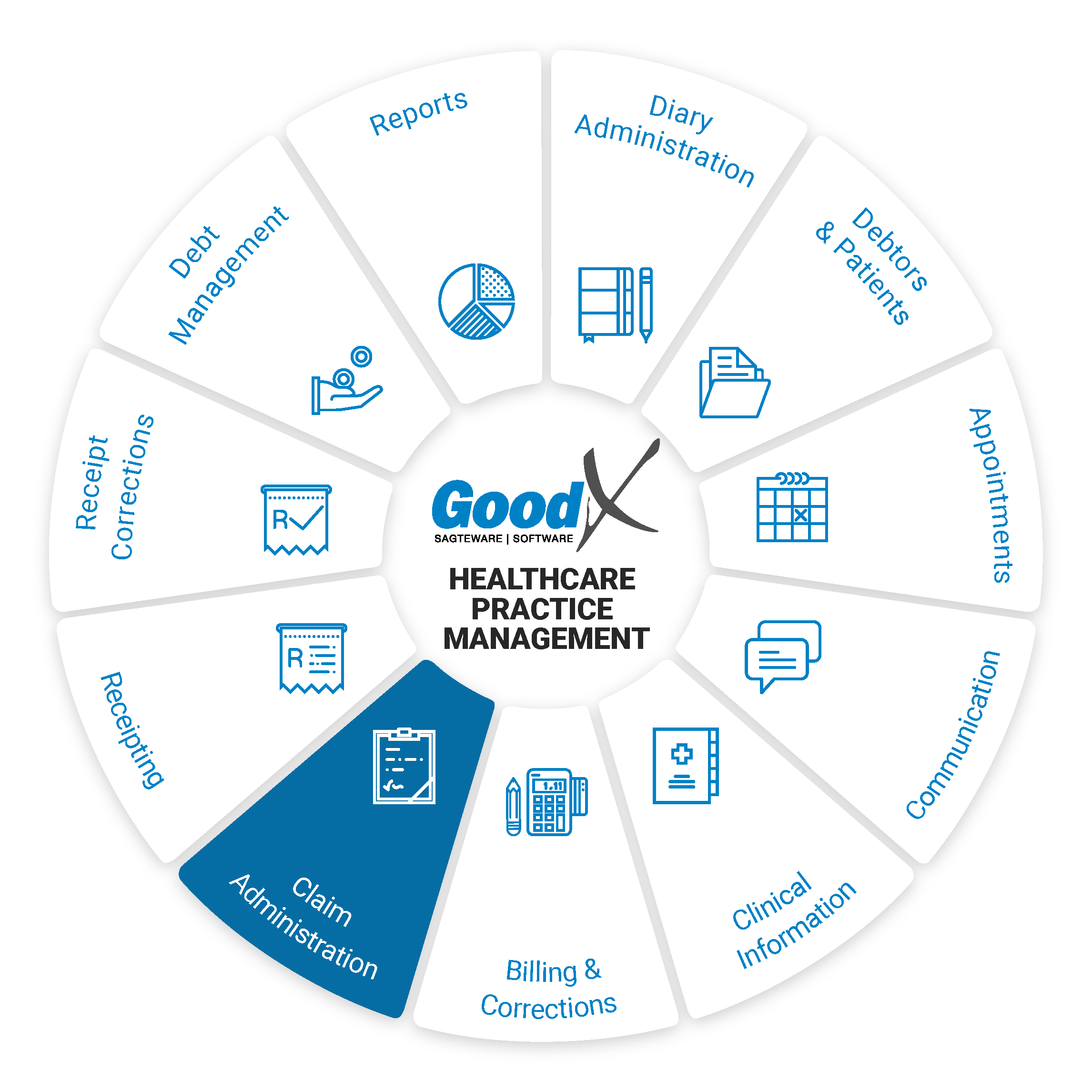
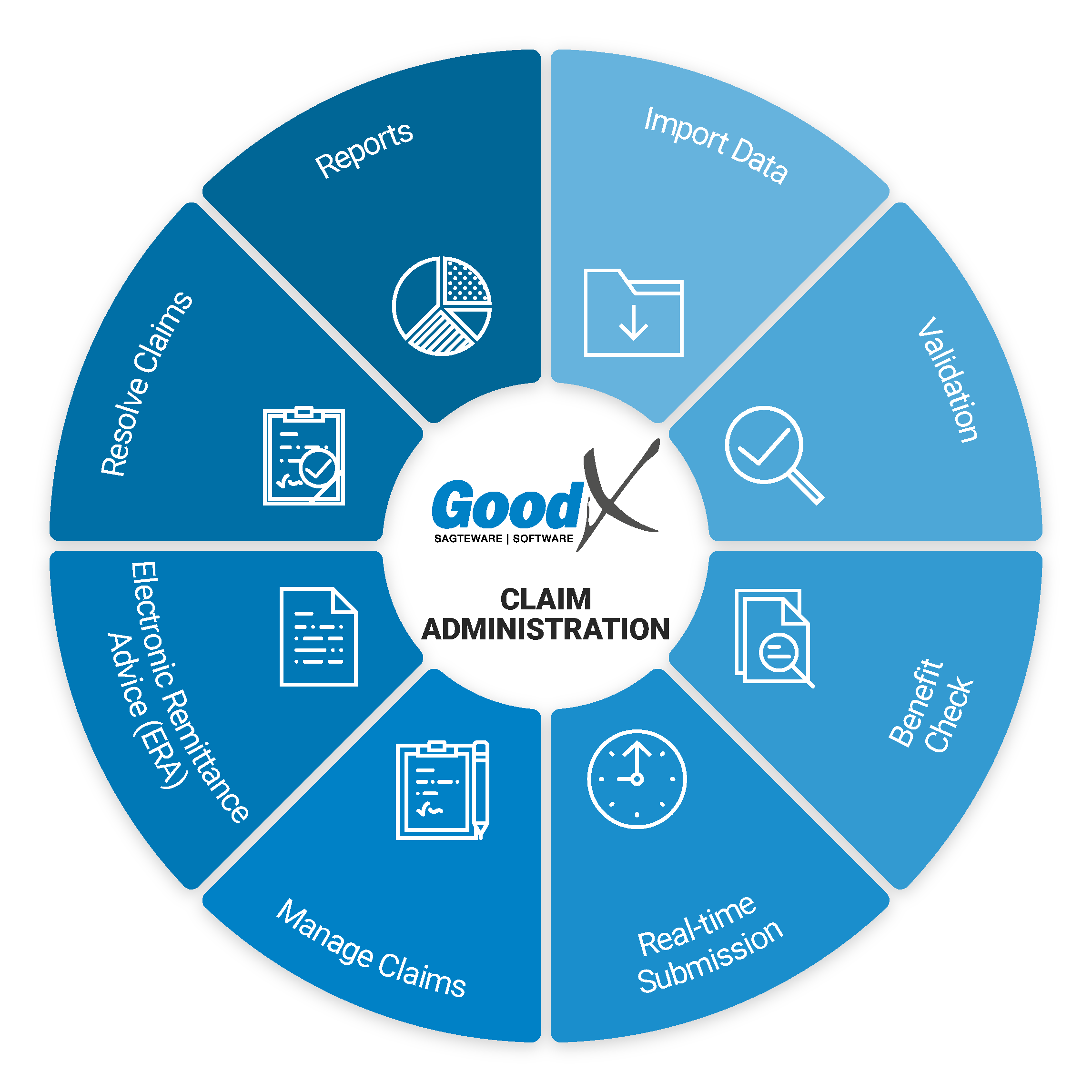
11. Claim Administration: Roles, Purpose & Business Diagram
Responsible Roles
 |
Management Role:
|
|---|---|
|
|
Operational Role:
|
|
|
Operational Role:
|
| Action maps: Collection stage:
|
 Purpose of Claim
Administration
Purpose of Claim
Administration
GoodX provides practice management software and switching integrated directly into GoodX Software. This means you can manage everything from GoodX Software.
- Cash flow is of vital importance to the health of a practice. One way of optimising the cash flow is to send your claim to the medical aid before the patient leaves the practice so that the cashier will know if the medical aid will settle the account in full.
- If the medical aid rejects the claim, the cashier can inform the patient immediately and receive payment directly from the patient before they leave the practice.
- Claim administration assists the Practice so that the Debt Management run smoothly.
- We are referring to the 4 R’s - Reverse, Redo, Resend, Resolve.
GoodX Switch allows you to submit claims directly and in real-time into all major medical aid computer systems and to receive proof of submission and delivery of claims directly into GoodX. The switch establishes communication to and from medical aids so that the practice can adequately administrate their claims.
Switching Partner - GoodX Switch
A switching partner is a system that sends medical aid claims to the medical aid and receives the response for the claim.
The switching partner will assist in electronically sending the claim (bill) of the patient's invoice. This will help see if the medical aid has received the claim and if the claim is correct, according to the response that will be received.
The response indicates that the claim will be paid, but this is not 100% proof that the claim will be paid. There can also be other reasons the medical aid will not pay a bill even if all the information on the claim is correct.
- Medprax updates:
- Routing codes of the medical aids for successful EDI.
- Discontinued medical aid plans
- Changed medical aid plans
- New medical aid schemes and plans
- Changed medical aid administrators
- Billing rules for medication and materials
- Medical Aid Enablement:
- Enabling medical aids in the system, real-time and non-real-time medical aids, where the switch is real-time and will give an immediate response or where it is non-real-time where the response is not immediate.
- Remember to run the medical enablement to update the new and changed medical aid plans or schemes and check that all new medical aids are linked to the correct price lists.
- The update report can be checked to see if the medical aid update was done correctly.
Cashflow Management
Good collection processes are vital to practice management to ensure healthy cash flow. Inadequate cash flow is often the result of mistakes ending up in rejections, and when rejected claims are not quickly followed up, it results
in claims that lapse.
The functions available in GoodX assist the practice to import information correctly into GoodX, resulting in spelling and typing mistakes being eliminated. The validation function confirms if patients are still members
of medical aids and can confirm if funds are available for the claims to be paid.
The fact that most medical aid claims can be sent in real-time results in confirmation if claims are accepted for payment before a patient leaves the practice.
Patients can then settle their accounts before leaving the practice.
GoodX provides a handy screen for the resolution of rejected claims. Claims can be corrected and resent to the medical aids without extra costs so that claims will not lapse.
Electronic remittance advice results in an easy and speedy allocation of payments, ensuring that debtor data is up to date for quick debt collection.