Best Practice Guidelines: Healthcare Practice Management & POPIA Compliance Framework
Best Practice Guidelines: Healthcare Practice Management
&
POPIA Compliance Framework
Copyright © 2021 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
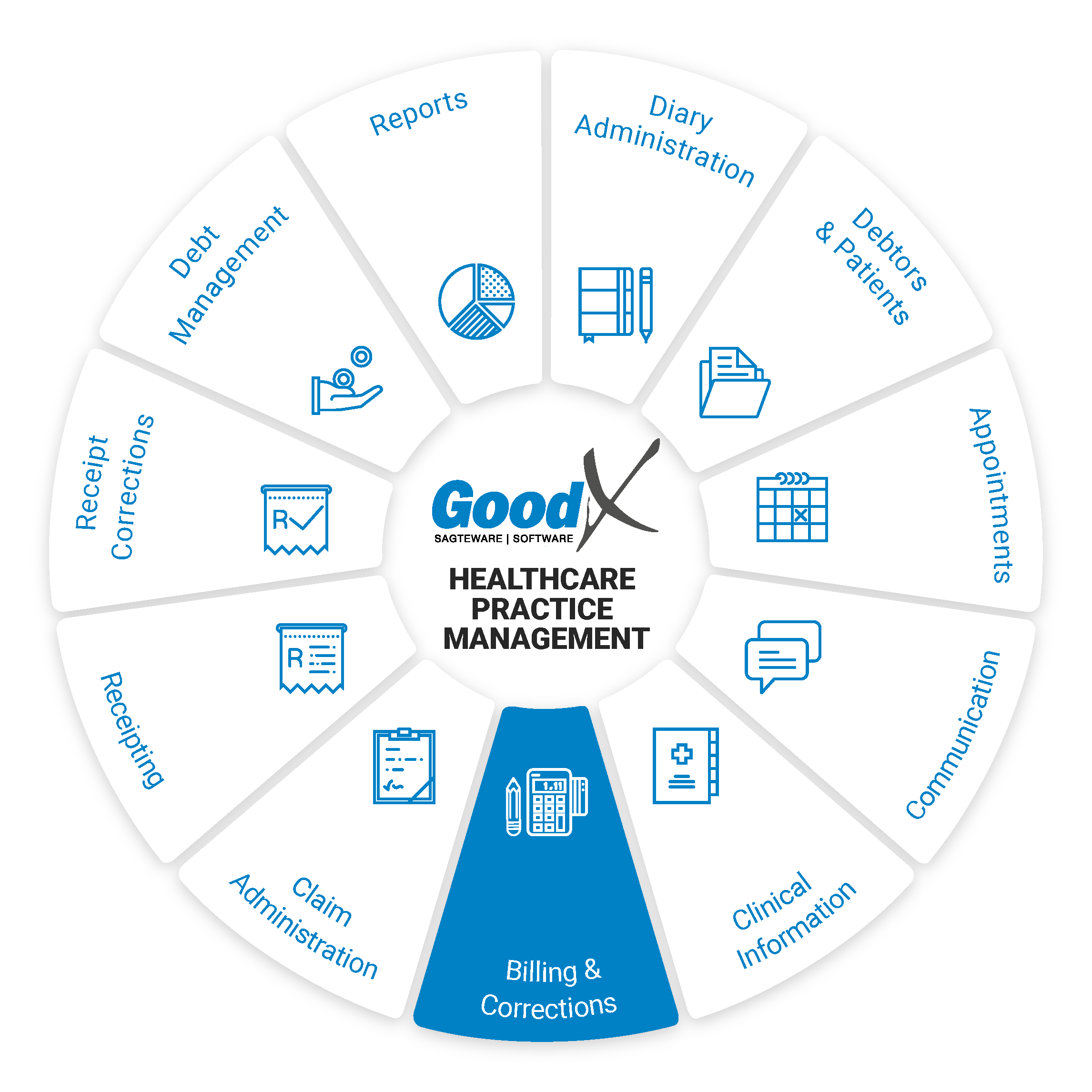
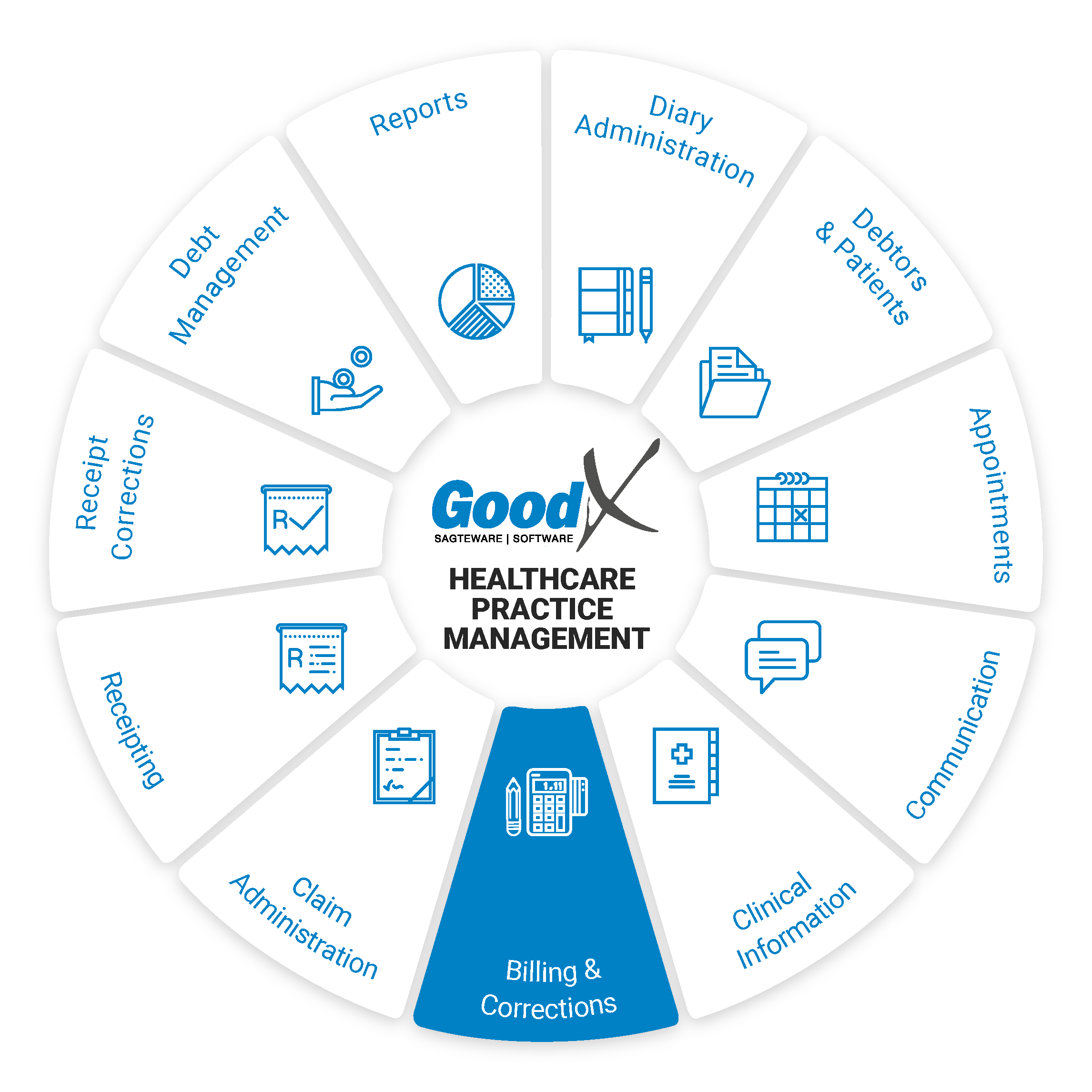
9. Billing: Roles & Purpose
Responsible Roles
 |
Operational Role:
|
|---|---|
|
|
Management Role:
|
|
|
Operational Role:
|
 |
Operational Role:
|
 |
Operational Role:
|
 |
Operational Role:
|
| |
Action maps: Collection stage:
Compliance continuity:
|
 Purpose
of Billing
Purpose
of Billing
Billing is equal to Income (money). Billing is the only way to generate income for the procedures that were done or stock that was used or sold. Billing ensures that timely, accurate and complete accounts are submitted to medical aids or issued to private
patients.
 Purpose
of Billing
Purpose
of BillingBilling ensures income into the practice to pay accounts and salaries. Patients need to be billed to get income into the practice. Without income, the practice will come insolvent. A practice stays a business that needs income to be able to keep on treating patients.
The billing chapter will be divided into the following sections:
- Optimisation of Turnover in your practice
- Tariffs and Terminology
- Medical codes and Rules
- Billing Business Processes
Billing vs coding
Medical billing and coding are the backbones of the healthcare revenue cycle, ensuring Medical Schemes, Insurers, and patients reimburse providers for services delivered. Medical billing and coding translate a patient encounter into the language of claims submission and reimbursement.
Billing and coding are separate processes, but both are crucial to receiving payment for healthcare services. Medical coding involves extracting billable information from the medical record and clinical documentation, while medical billing uses those codes to create claims and bills for patients. Creating claims is where medical billing and coding intersect to form the backbone of the healthcare revenue cycle.
The process starts with patient registration and ends when the provider receives full payment for all services delivered to patients.

