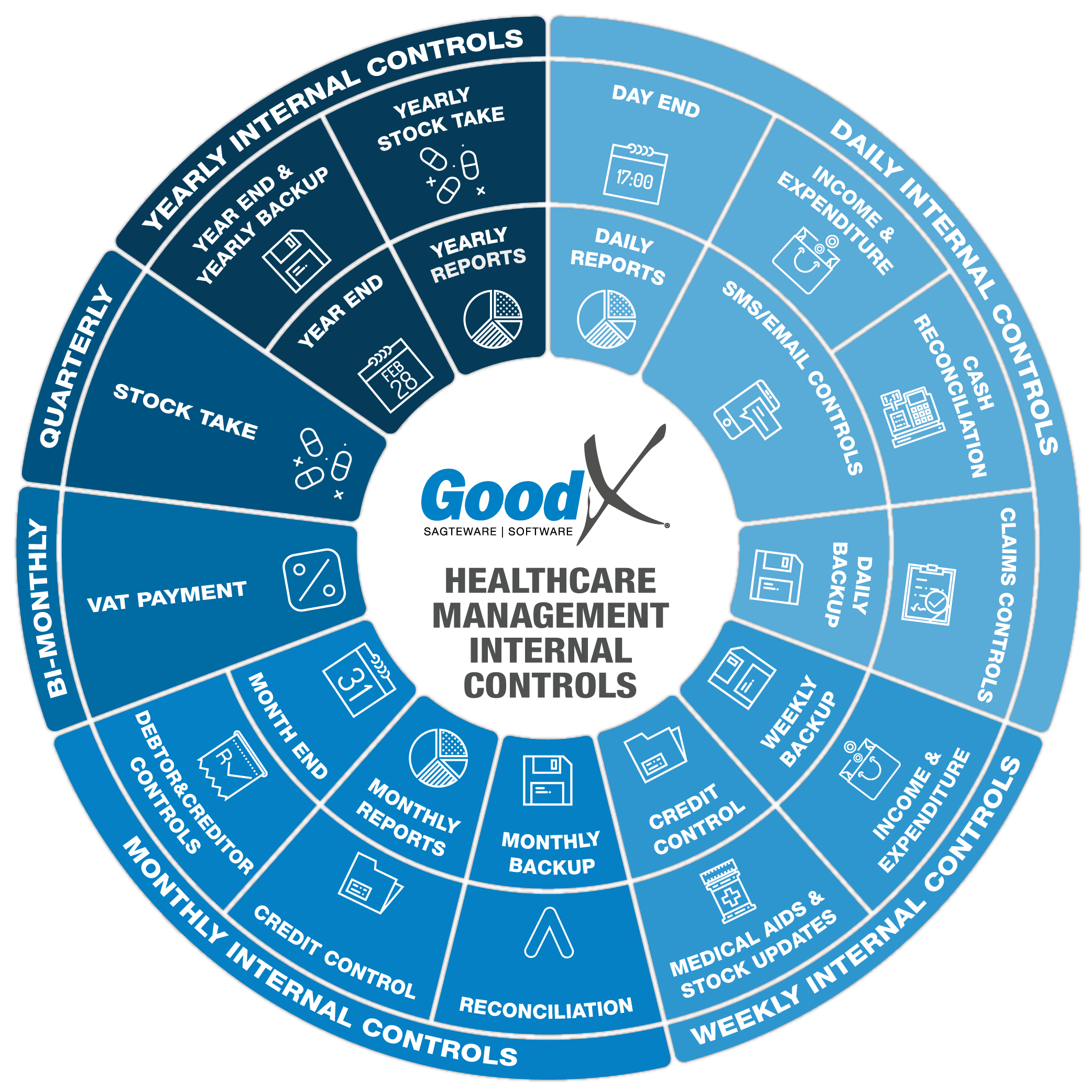
Best Practice Guidelines: Healthcare Management Internal Controls
Best Practice Guidelines: Healthcare Management Internal Controls
Copyright © 2020 GoodX Software. All rights reserved.
GoodX online Learning Centre
learning.goodx.co.za
2. Daily Internal Controls Summary
2.4. Claims Controls
Claims controls are performed on all medical aid payable invoices that have been switched to the medical aids. It is important to make sure that the claims are checked daily for the following reasons:
- To ensure payments from the medical aids are on time so that there will be sound cash flow.
- Ensure that all claims are submitted to the medical aids before they become stale, which is 3 to 4 months from the service date.
- To move any outstanding or rejected claims to the patient-liable account so that patients can pay any outstanding amounts.
- Utilising the validation and import functions to ensure more accepted claims and fewer rejections due to wrong demographic data.
On the Claim History screen, the practice manager will be able to view all claims that have been submitted to the medical aids that have not been resolved. Filters can be used to only view claims for a specified period. This function informs the management of all rejected claims on a daily basis. Claims can be amended and resent to make sure they don't become stale.
The 4 R's
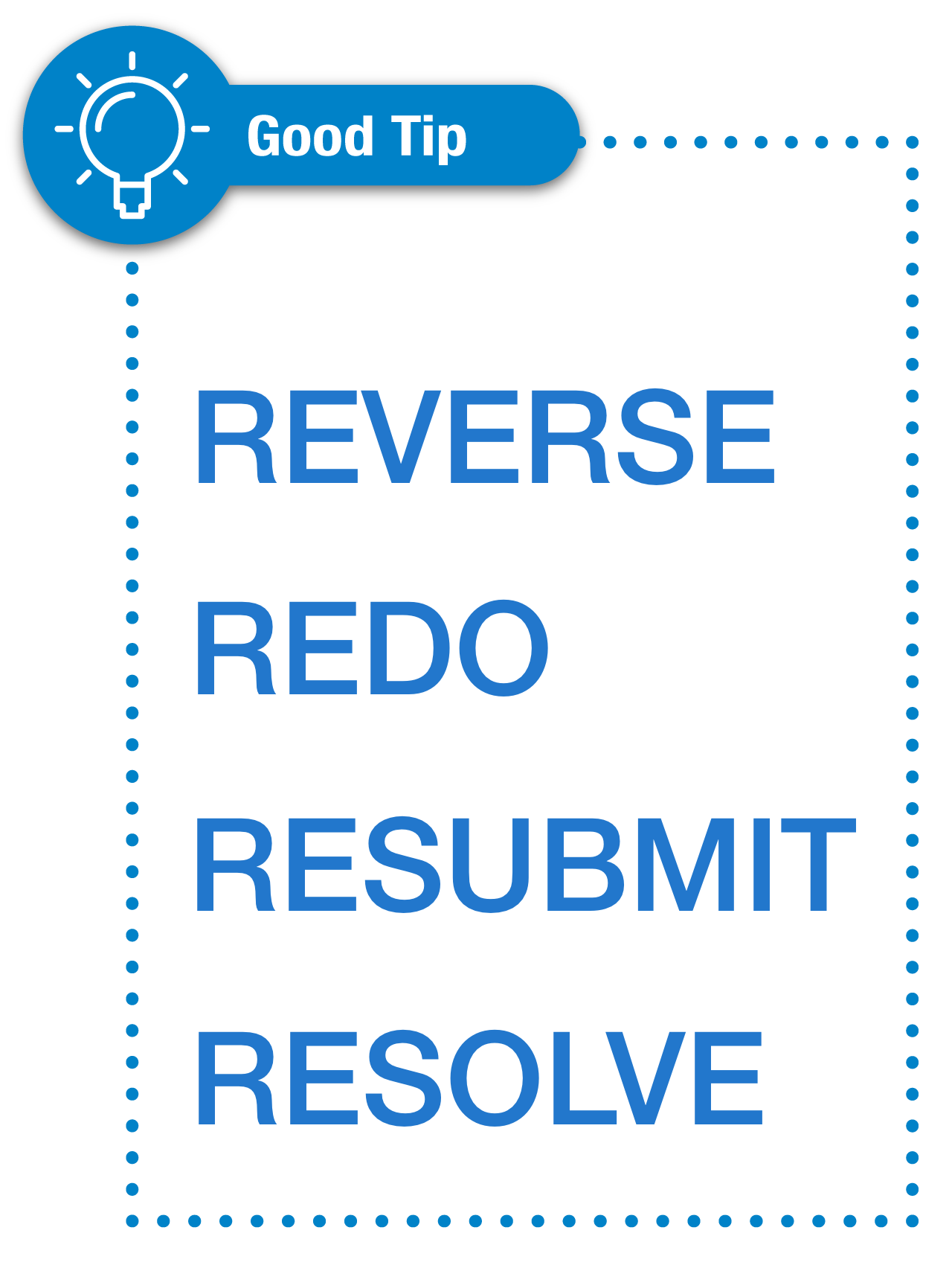
When dealing with claims that were rejected by medical aids, amendments must be made as soon as possible to avoid financial loss. It is easy to remember the 4 R's that need to be done to fix claims:
- Reverse - a claim must always first be reversed before any corrections can be made.
- Redo - correct vital mistakes on claims like codes and amounts.
- Resubmit - resend amended claims or not received claims to the medical aid.
- Resolve - mark the claim as resolved if everything is correct and the claim is marked as approved by the medical aid.

GoodX Switch Claim History Screen
The screen shows all claims submitted to the medical aids with their switch status, references and amounts.
- Make sure there are no delayed responses.
- Check the "EDI Status" to see if the claims were successful.
- Resubmit any "Error" claims.
- Ensure all "To Send" claims have been resubmitted.
- Look at the "EDI Status" for None claims that should have been submitted.
- Investigate any Item level rejections.
- Investigate any warning messages on the claims.
- Investigate all the rejected claims.
- Reverse, Redo and Resubmit incorrect/rejected claims.
- Confirm that claims are marked as Resolved if the claims were processed successfully or have been resubmitted (Electronic or paper claim).
Resolve function
Resolving claims takes them off the to-do list and thereby assists the user to only work on claims that need user input for corrections or follow-up.
There are two basic ways that practices use the resolve function:
- Resolving claims as soon as the medical aids confirm acceptance of the claims - no further user input is needed for the submissions and these practices will use the credit control assistant to do credit control;
- Resolving claims when full payment has been received by the medical aids or patients - these practices use the claims history screen as part of their credit control process.
The goal of the claim history screen is to make sure all claims have been resolved and everything was done to ensure that the medical aids are going to, or paid the claim.